RECOMMENDATION: Molnupiravir should not be used routinely for treatment of COVID-19. It may be considered as an option when remdesivir or nirmatrelvir-ritonavir (Paxlovid) are not available or appropriate, for patients with mild to moderate COVID-19 illness of less than 5 days’ duration, in patients with risk factors for severe disease (see Justification).
DATE OF RECOMMENDATION: 04th April 2024
Definition of mild:
• Symptomatic (any acute COVID-19 related symptoms)
• AND respiratory rate <24/min
• WITHOUT pneumonia or hypoxia
Definition of moderate illness:
• Pneumonia (clinical or radiological) OR hypoxia (SpO2 <94% in adults with no underlying lung disease)
• AND respiratory rate ≤30/min
• AND SpO2 ≥90% on room air
Definition of Severe illness
Pneumonia with ANY ONE of the following:
• severe respiratory distress or respiratory rate >30/min
• SpO2 <90% on room air
• NO invasive or non-invasive respiratory support needed
Definition of critical:
• Requirement for high-level respiratory support: noninvasive ventilation, high-flow oxygen (≥20 litres per minute) or invasive mechanical ventilation
• OR acute respiratory distress syndrome (PaO2/FiO2 ratio of <300)
• OR sepsis
• OR shock
A conditional recommendation is one for which the desirable effects probably outweigh the undesirable effects (weak recommendation FOR an intervention) or undesirable effects probably outweigh the desirable effects (weak recommendation AGAINST an intervention) but appreciable uncertainty exists. This implies that not all will be best served by this recommendation and decisions can be made by the patient and caregiver based on patient values, resources and setting with a clear understanding of the ensuing harms and benefits.
Definition of mild:
• Symptomatic (any acute COVID-19 related symptoms)
• AND respiratory rate <24/min
• WITHOUT pneumonia or hypoxia
Definition of moderate illness:
• Pneumonia (clinical or radiological) OR hypoxia (SpO2 <94% in adults with no underlying lung disease)
• AND respiratory rate ≤30/min
• AND SpO2 ≥90% on room air
Definition of Severe illness
Pneumonia with ANY ONE of the following:
• severe respiratory distress or respiratory rate >30/min
• SpO2 <90% on room air
• NO invasive or non-invasive respiratory support needed
Definition of critical:
• Requirement for high-level respiratory support: noninvasive ventilation, high-flow oxygen (≥20 litres per minute) or invasive mechanical ventilation
• OR acute respiratory distress syndrome (PaO2/FiO2 ratio of <300)
• OR sepsis
• OR shock
Molnupiravir is the first oral antiviral developed for treatment of COVID-19 by Merck, Sharp and Dohme and Ridgeback therapeutics1. In November 2021 it was granted conditional authorization by Britain for use in mild to moderate COVID-19 infection2. In December 2021, FDA granted emergency use authorization for treatment of mild COVID-19 infection3.
Very low certainty evidence from randomised controlled trial data suggests that Molnupiravir may have an uncertain effect on the risk of hospitalisation or death (very low certainty evidence). Low certainty evidence also suggests that it may have little to no effect on all cause mortality or clinical improvement at day 28 and may lead to a negative PCR for SARS-CoV-2 at day 7.
Remdesivir and Nirmatrelvir/ritonavir are antivirals with stronger evidence for efficacy and safety. Considering uncertainties about safety and the risk of resistance, Molnupiravir should not be used as a first-line option for patients at risk of hospitalisation. However, for patients at high risk of hospitalisation, where Remdesivir and Nirmatrelvir/ritonavir are not available, or cannot be used due to drug-drug interactions, or intravenous therapy is deemed inappropriate, Molnupiravir may be an alternative option. Risk factors for hospitalization include immunocompromise, obesity, diabetes and/or chronic cardiopulmonary disease, chronic kidney or liver disease, active cancer, those with disabilities, and people who have not been vaccinated against SARS-CoV-2.1
Date of latest search: 01st March 2023
Date of completion & presentation to the Expert Working Group: 25th January 2024
Date of planned review:
Evidence Synthesis Team: Hanna Alexander, Jane Miracline, Hana Nazim, Naveena Gracelin Princy Z, Priscilla Rupali
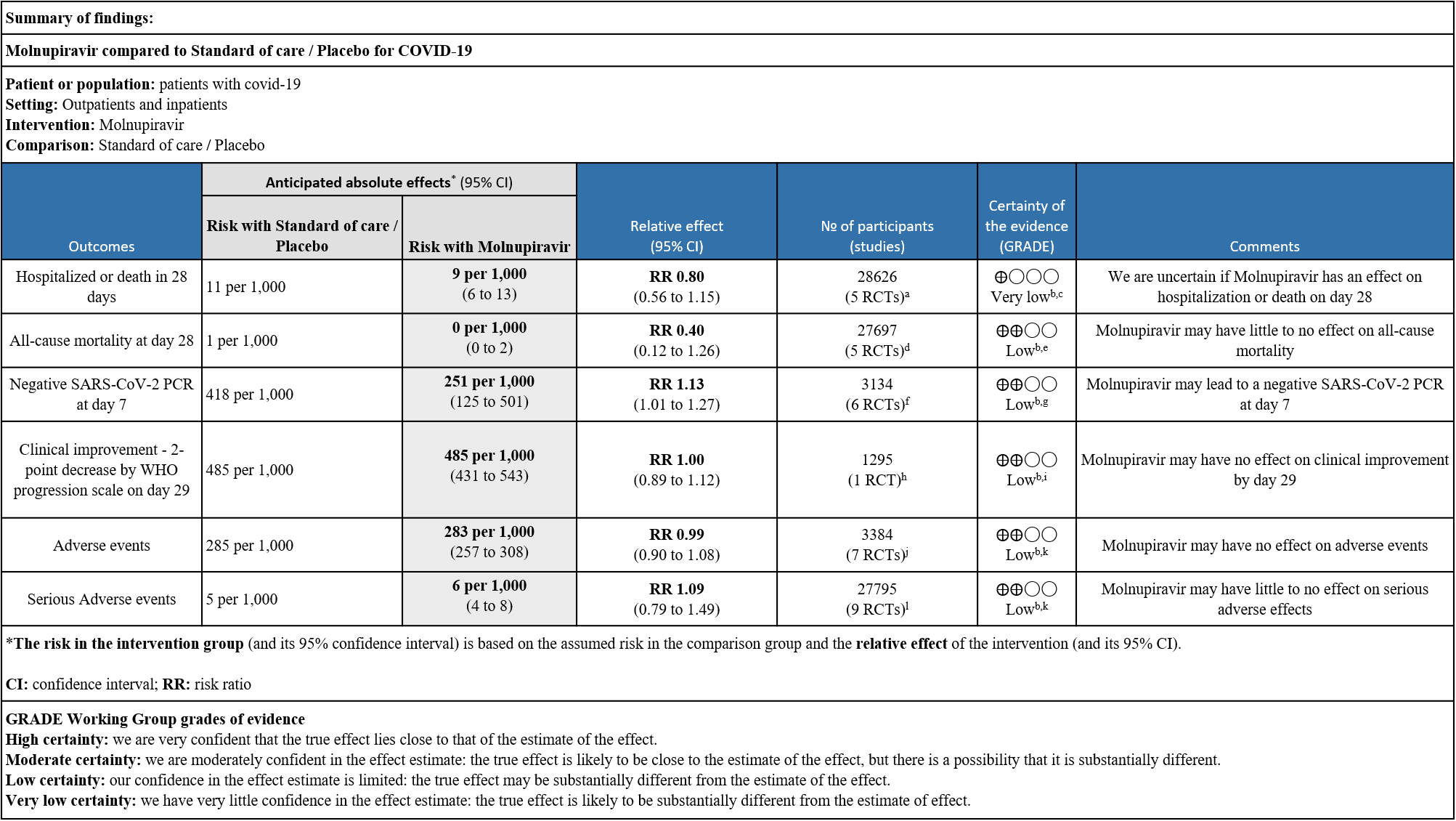
Explanations:
a. Bernal,Bulter C, Caraco Yosef, Khoo, Thippabotta
b. Downgraded by one level for serious indirectness as the study population includes unvaccinated participants which does not reflect the current scenario
c. Downgraded by two level for serious imprecision as the lower bound of the 95% CI includes appreciable benefit and the upper limit includes harm
d. Aribas, Bernal, Bulter C, Caraco Yosef, Fischer
e. Downgraded by one level for serious imprecision as the upper CI limit represents harm and the event is very rare
f. Bernal, Bulter C, Fischer, Khoo, Thippabotta, Zou R
g. Downgraded by one level for inconsistency as we identified substantial heterogeneity (I2=63%)
h. Bernal
i. Downgraded by one level for serious imprecision: lower confidence interval, bound represents a mild benefit from Molnupiravir whereas the upper bound includes harm
j. Aribas, Bernal, Caraco Yosef, Fischer, Khoo, Thippabotta, Zou R
k. Downgraded by one level for serious imprecision as the lower bound of the 95% CI includes appreciable benefit and the upper limit includes harm
l. Aribas, Bernal, Buter C, Caraco Yosef, Fischer, Khoo, Kumarasamy, Thippabotta, Zou R
Molnupiravir was the first oral antiviral treatment developed specifically for COVID-19 developed by Merck, Sharp and Dohme and Ridgeback Therapeutics. Molnupiravir is a newer orally bioavailable prodrug of Emory Institute of Drug Development-2801 [EIDD-2801]/MK-4482), which is the synthetic ribonucleoside derivative N4-hydroxycytidine and ribonucleoside analog, with potential antiviral activity against a variety of RNA viruses recently been tested for COVID-19. The TP form of EIDD-1931 is incorporated into RNA and inhibits the action of viral RNA-dependent RNA polymerase. This results in the termination of RNA transcription, decreases viral RNA production, and viral RNA replication2. In November 2021, the UK authorised Molnupiravir for use in people who have mild to moderate COVID-19 and at least one risk factor (such as obesity, older age, diabetes mellitus or heart disease) for developing severe illness3. The FDA granted emergency use authorization for the treatment of mild COVID-19 infection in December 20214. With the advent of different covid variants, the monoclonal antibodies which were useful antivirals in mildly symptomatic or asymptomatic individuals who were at high risk of severe COVID-19 infection rapidly became ineffective5. Hence oral options like molnupiravir and Nirmatrelvir/ritonavir became attractive options. However, controversy remains regarding the utility of Molnupiravir with widespread vaccination globally thus reducing risk of severe disease in high risk patients. The drug though invented at Emory University was later acquired by Ridgeback therapeutics in partnership with Merck & Co, USA. Molnupiravir was initially developed as a possible treatment for influenza viruses, encephalitic alphaviruses like Venezuelan, Eastern and Western equine encephalitic viruses due to its significant inhibitory effect in cell cultures6. On December 23rd 2021 FDA gave emergency use authorization for the treatment of mild-to-moderate coronavirus disease (COVID-19) in adults (>18yrs) with who are at high risk for progression to severe COVID-19, including hospitalization or death, and for whom alternative COVID-19 treatment options were are not accessible or clinically appropriate. An in-vitro study by Zhou et al has suggested that the drug, though intended to disrupt only viral RNA, could also incorporate into and cause mutations in human DNA and potentially “contribute to the development of cancer”. Molnupiravir metabolite the ribonucleoside analog β-D-N4 -hydroxycytidine (NHC), is a potent mutagen.
However, even with the advent of new strains with immune escape, Molnupiravir retains its activity against the VOCs Alpha, GHB-03021/2020* and Omicron, making this a possible therapeutic option. This review aims to update the evidence from randomized clinical trials of Molnupiravir for treatment of COVID-19, for any duration, which could guide clinicians and researchers regarding the appropriate use of this drug.
We searched PubMed, Epistemonikos, and the COVID‐19‐specific resource www.covid‐nma.com, for studies of any publication status and in any language. We also reviewed reference lists of systematic reviews and included studies. We performed all searches up to 01st March 2023.
We searched the above databases and found 25 records. After removing duplicates and excluding studies that did not match our PICO question, 9 RCTs were included in the review.
We extracted data for the following outcomes, pre-defined by the Expert Working Group:
PICO:
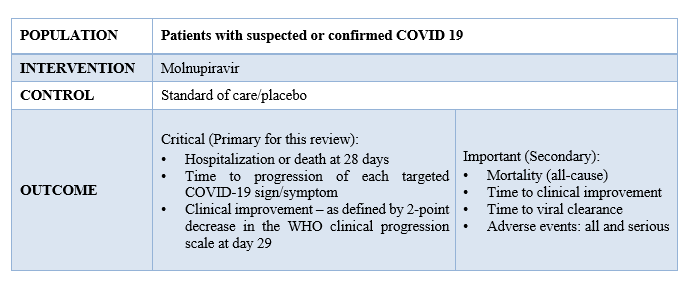
Two reviewers independently assessed eligibility of studies from the search results using the online Rayyan tool. Data extraction was performed by one reviewer, and checked by another, using a piloted data extraction tool. Risk of bias (RoB) was assessed using the Cochrane RoB v2.0 tool, with review by a second reviewer and compared with covid.nma database. If there was a difference in more than one domain it was assessed by a third independent author. We used risk ratios (RR) for dichotomous outcomes and mean differences (MD) for continuous outcomes, with 95% confidence intervals (CIs). We performed a meta-analysis if outcomes were measured and reported in a similar way for the populations in each trial using random-effects models with the assumption of substantial clinical heterogeneity and the I2 test to calculate residual statistical heterogeneity, using Review Manager (RevMan) v5.4. Evidence would then be synthesized and reviewed by the Methodology Committee. We considered use of fixed effects model if we found that adequate weightage was not given to bigger trials on advice from the methodology committee. We used GRADE methodology to prepare summary of findings tables on GRADEPro GDT.
We found 9 RCTs that matched the PICO question as pre-defined by the expert working group.
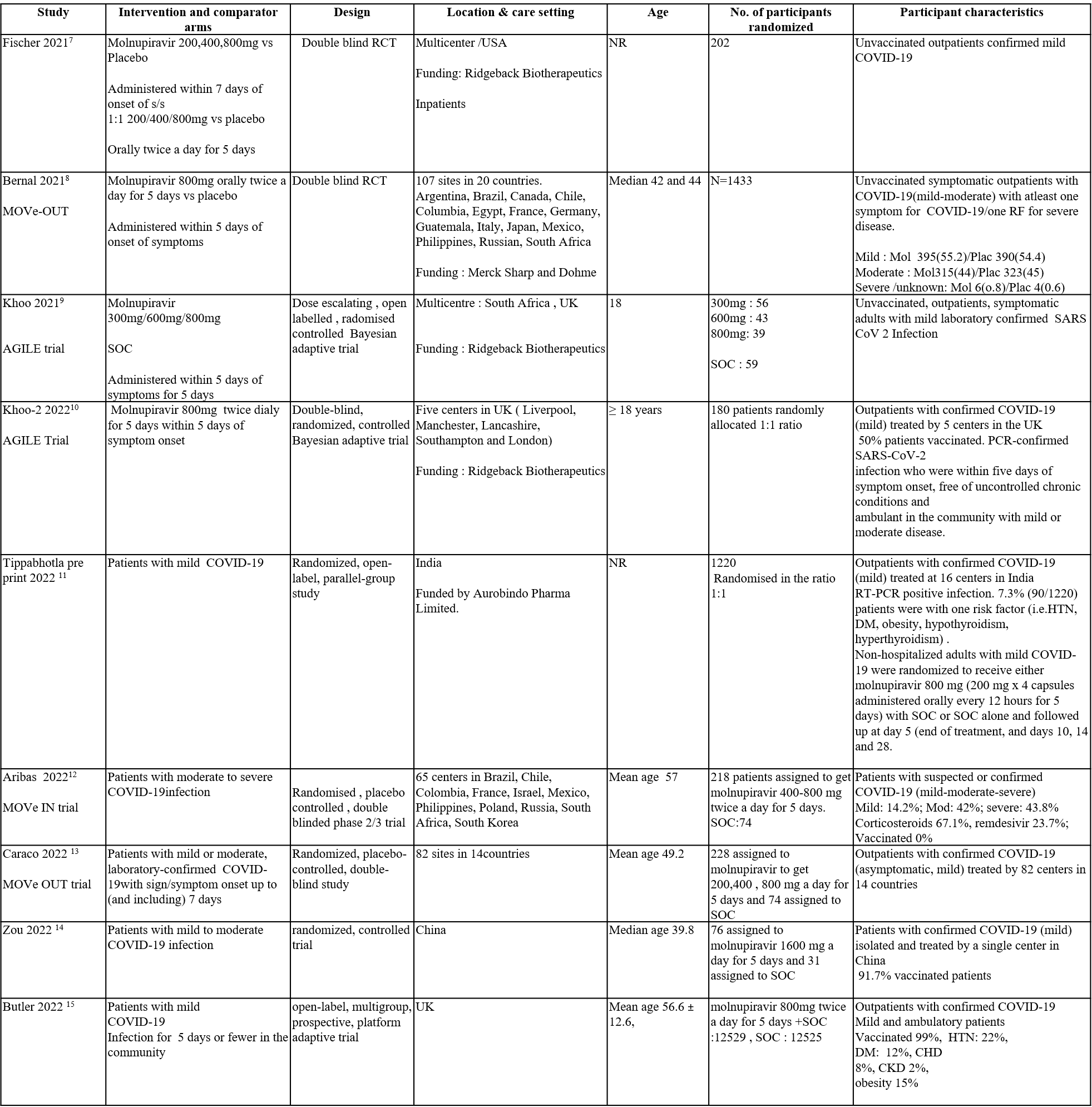
Apart from the 3 trials we included in the previous recommendation, we have included 6 more trials for the evidence update. The trials included a total of 29725 participants, all of whom were adults. Three trials were a multicenter trials involving many countries like Brazil, Chile, Colombia, France, Israel, Mexico, Philippines, Poland, Russia, South Africa, and South Korea. Two trials reported from UK, one from India and one from china. Four trials included unvaccinated patients and three trials had 50-60% of population, vaccinated. One trial had 99% of its population vaccinated. Four trials compared Molnupiravir with placebo whereas the other five trials compared Molnupiravir with standard of care.
Each trial and its results are described below, characteristics of the trials are summarized in the Summary of characteristics of included trials table. Risk of bias for each outcome as per domain in each trial is displayed alongside the forest plots below. The following comparisons were investigated in the trials (we compared outcomes for arms randomized to Molnupiravir vs. standard of care or placebo).
- Six trials compared Molnupiravir with placebo (2606 participants).
- Three trials compared Molnupiravir with standard of care vs Standard of care alone (27119 participants).
Our expert working group classified the following outcomes as critical - hospitalization or death in 28 days, time to progression of each targeted COVID-19 sign/symptom, clinical improvement –as defined by 2-point decrease in the WHO clinical progression and mortality (all-cause), time to clinical improvement, time to viral clearance, Adverse events: all and serious as important outcomes.
Outcomes
As presented in the ‘Summary of Findings’ table, the effect of Molnupiravir on mortality, negative SARS-CoV-2 PCR at day 7, clinical improvement, adverse events and serious adverse events is of low certainty. In addition, the effect of Molnupiravir on hospitalized or death at 28 days was found to be very low quality evidence.
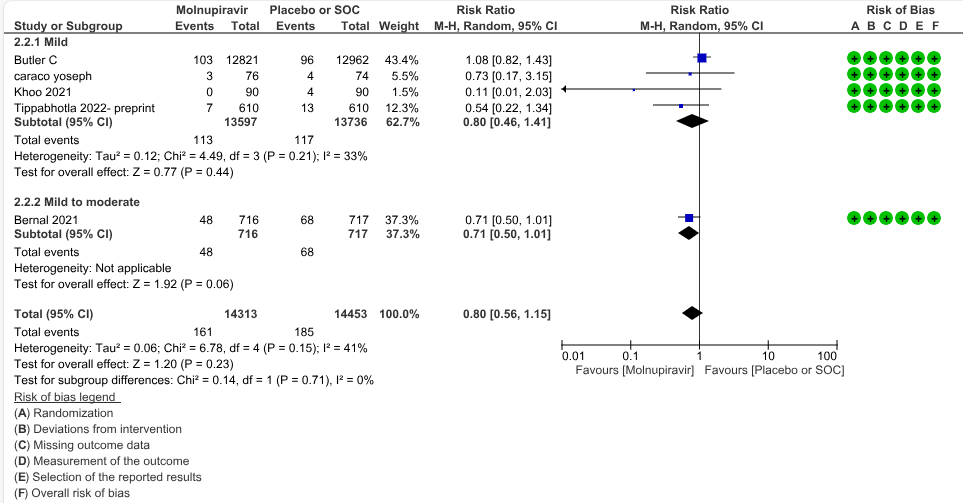
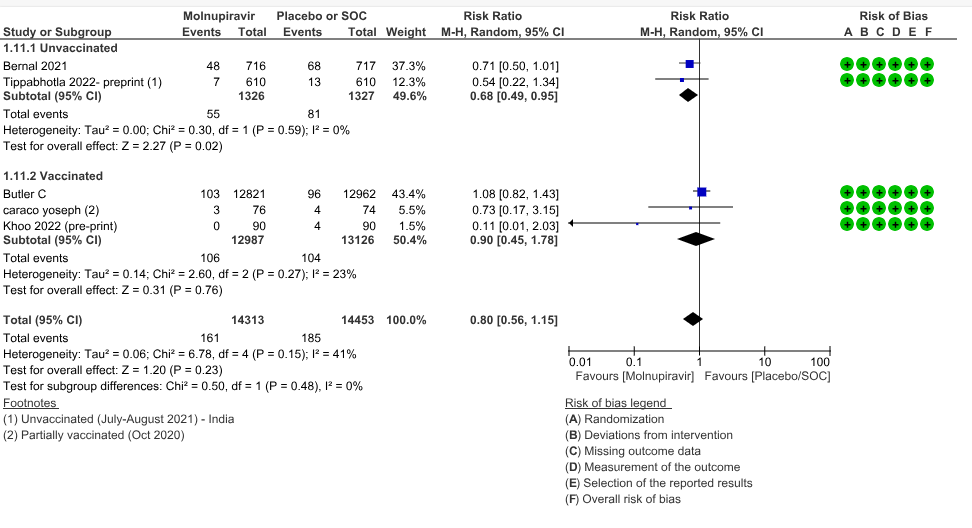
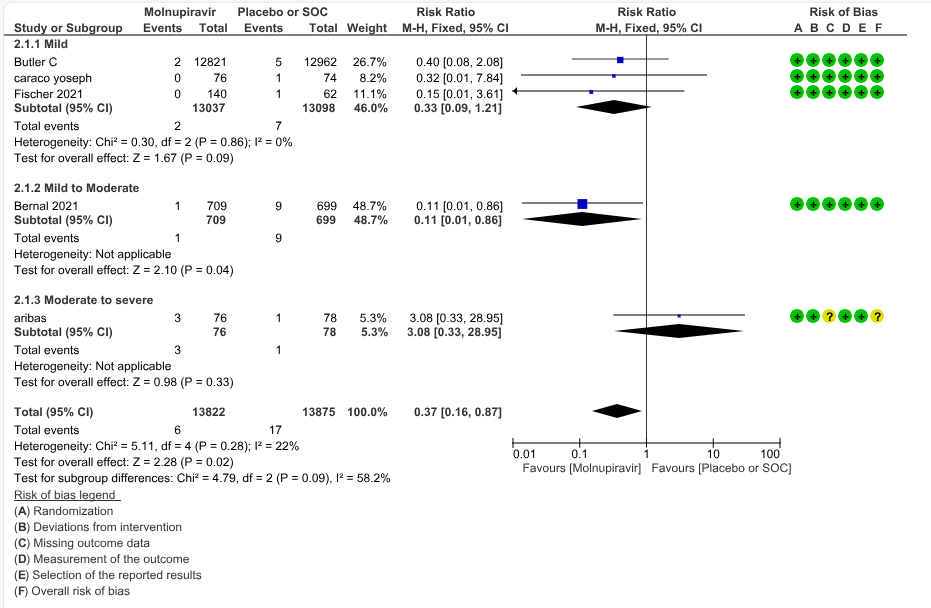
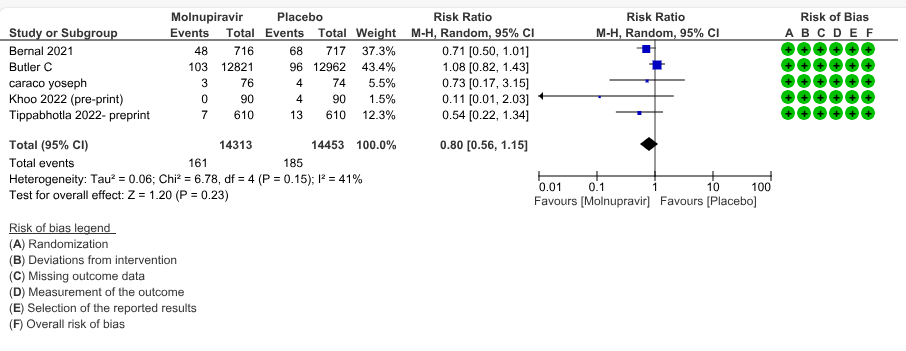
a. Hospitalized or death in 28 days: Very low certainty evidence in 5 trials with 28766 patients revealed that Molnupiravir has uncertain effect on hospitalization or death in 28 days compared to standard of care or placebo. However, there was a wide confidence interval, ranging from important benefit to important harm (RR 0.80; 95% CI 0.56 to 1.15, I2=41%).
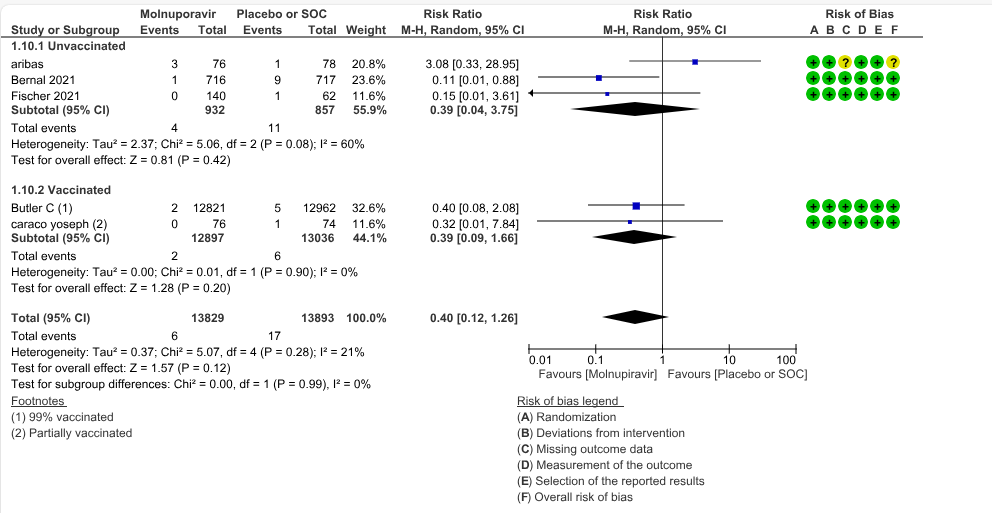
b. All-cause mortality: Low certainty evidence in 5 trials with 27697 patients suggested that Molnupiravir may have little to no effect on all-cause mortality compared to placebo or standard of care. We used a fixed effect model for this meta-analysis to give appropriate weightage to the larger trials suggesting benefit (RR 0.40; 95% CI 0.12 to 1.26, I2=21%)
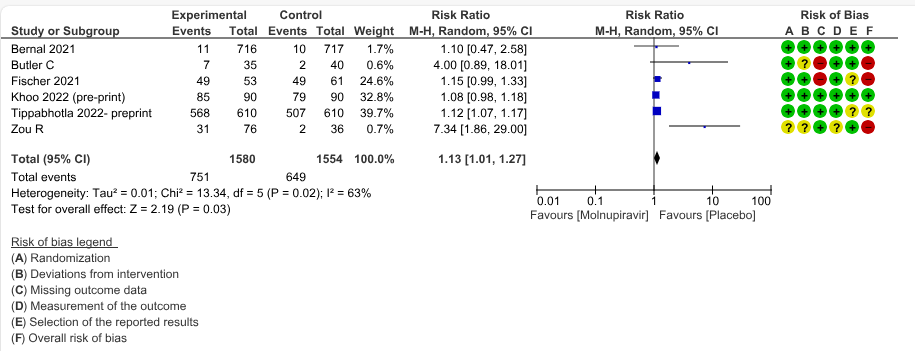
c. Negative SARS-CoV-2 PCR at day 7: Low certainty evidence in 6 small trials with 3134 patients revealed that Molnupiravir may lead to a negative SARS-CoV-2 PCR at day 7 (RR 1.13; 95% CI 1.01 to1.27, I2=63%).
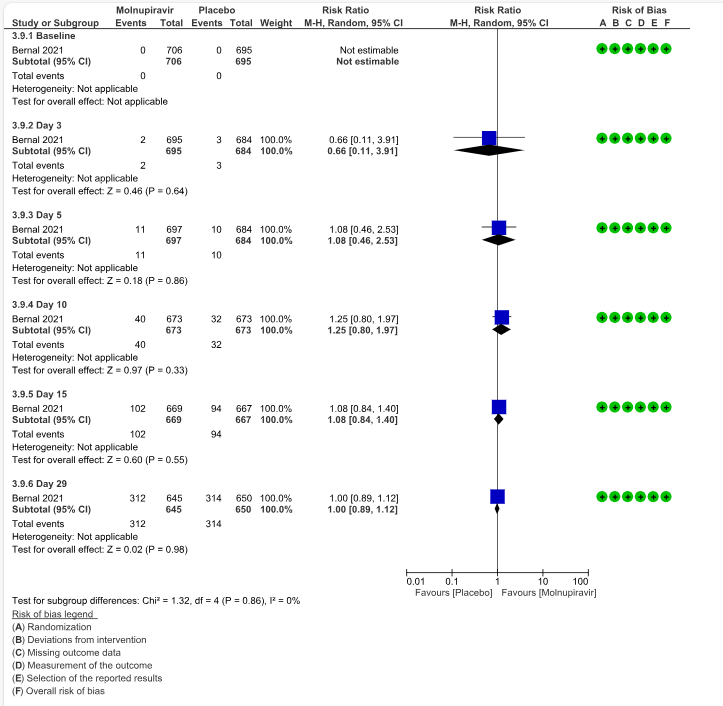
d. Clinical improvement – 2-point decrease by WHO progression scale by day 29: Low certainty evidence in one trial with 1295 patients suggested that Molnupiravir has no effect on clinical improvement by day 29 (RR 1.00; 95% CI 0.89 to 1.12, I2=0%).
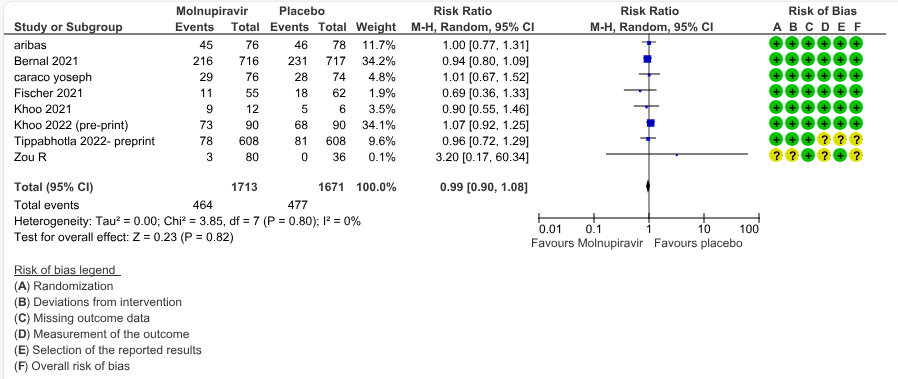
e. Adverse events: Low certainty evidence in 7 trials with 3384 patients suggested that Molnupiravir has no effect on adverse events compared to those receiving placebo or standard of care. (RR 0.99; 95% CI 0.90 to 1.08, I2=0%).
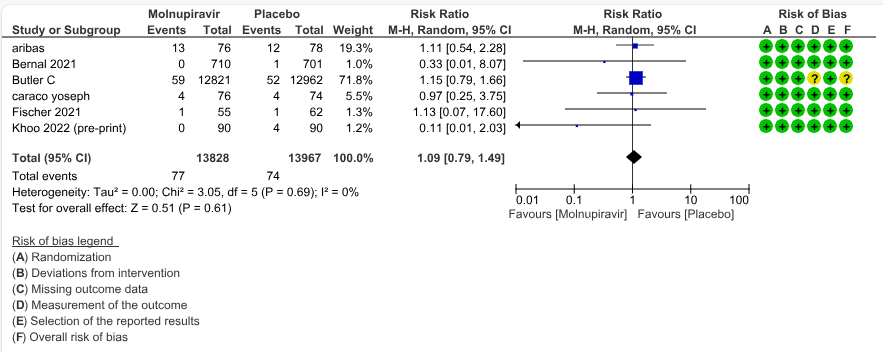
f. Serious Adverse events: Low certainty evidence in 9 trials with 27795 patients revealed that Molnupiravir may cause little to no effect on serious adverse effects in those receiving placebo or standard of care (RR 1.09; 95% CI 0.79 to 1.49, I2=0%).
1. Hospitalization or death at 28 days
Based on Severity
Based on vaccination status
2. All-cause mortality at day 28
Based on Severity
Based on Vaccination Status
1.Hospitalization or death by day 28
2. All-cause mortality D28
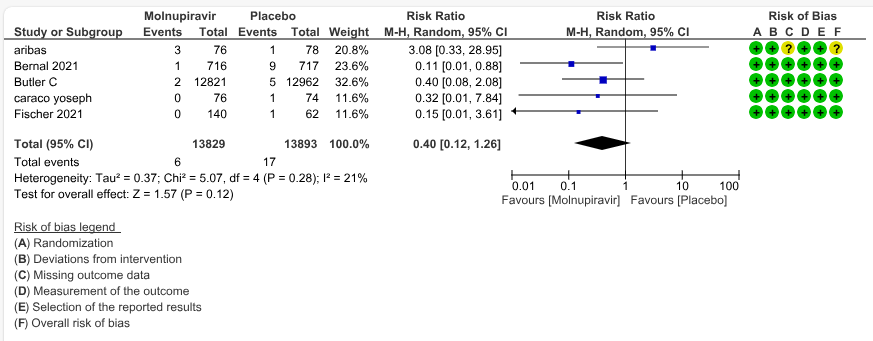
Sensitivity - Fixed Effect Analysis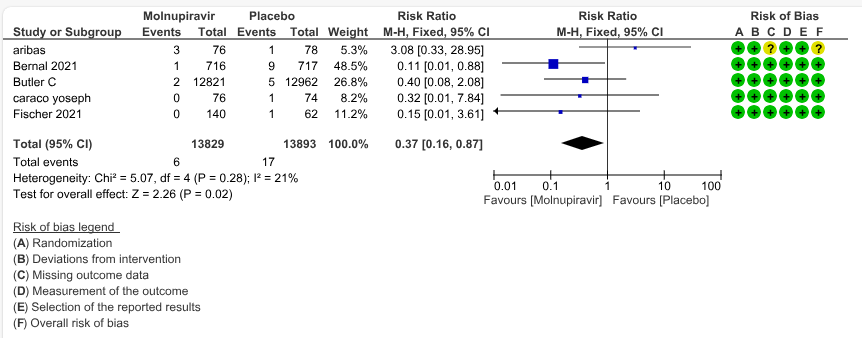
3. Negative SARS-CoV-2 PCR at Day 7
4.Clinical improvement scale 1-3 to 0 at Day 29
5. Adverse events
6.Serious adverse events
The Expert Working Group met on 25th January 2024 to update the recommendation for Molnupiravir as a treatment for COVID-19. Conflict of interest declarations were reviewed by the Steering Committee; none were found to be relevant to Molnupiravir.
Summary of Judgments
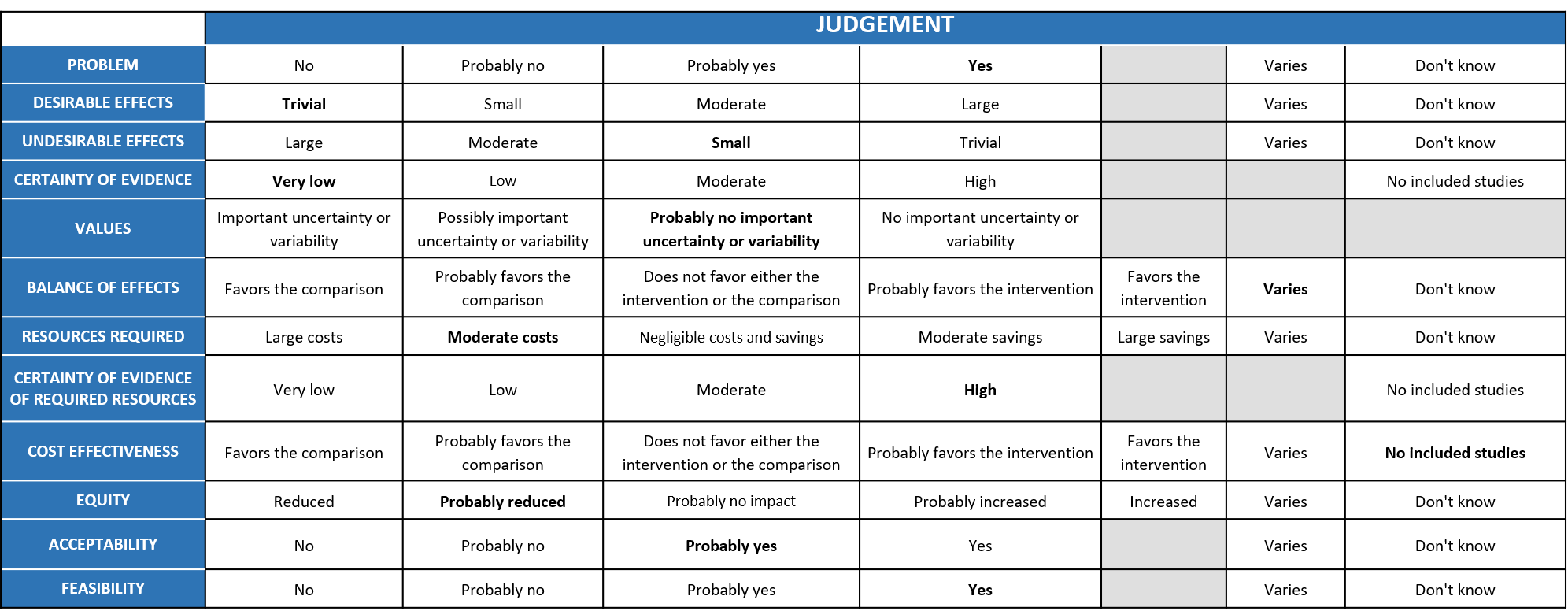
Problem
COVID-19 pandemic caused by the SARS-COV2 virus has significantly impacted India’s health structure by increasing the morbidity and mortality. Even though around 75% of the population is currently fully or partially vaccinated, limited antivirals are available for appropriate treatment. The group judged the problem to be of the utmost priority. This antiviral acts on RdRp, but differs from remdesivir. While remdesivir causes chain termination of SARS-CoV-2 virus, Molnupiravir causes mutagenesis of the virus or ‘error catastrophe’ during transcription, thus killing the virus.
Desirable effects
Very low certainty evidence from studies revealed that the effect of Molnupiravir is uncertain on hospitalization or death at 28 days RR 0.80 (95% CI 0.56 to 1.15) and may have little to no effect on all-cause mortality RR 0.40 (95% CI 0.12 to 1.26) with significant effect on conversion to negative PCR at Day 7 RR 1.13 (95% CI 1.01 to 1.27). The group voted that the overall desirable effects as trivial.
Undesirable effects
According to the data from studies, Molnupiravir may have no effect on adverse events RR 0.99 (95% CI 0.90 to 1.08) or serious adverse events RR 1.09 (95% CI 0.79 to 1.49). The group felt that the pooled data suggested that Molnupiravir was associated with little to no significant impact on adverse events, including serious adverse events. The group voted that the overall undesirable effects as small.
Certainty of Evidence
Using GRADE methodology, the evidence synthesis team rated the certainty of evidence as very low for hospitalization or death and low for all-cause mortality D28, Clinical improvement scale 1-3 to 0 Day 29, Incidence of PCR negativity by D7, serious adverse events and adverse events. The expert working agreed with these judgements and rated the overall certainty of evidence as low.
Values
The panel discussed the following points and concluded that there is probably no important uncertainty or variability.
Balance of effects
Earlier, since the studies have looked at unvaccinated population with mild to moderate disease across the studies, the panel felt that it is not representative of the current scenario. But in this review studies included vaccinated populations like Zou, Butler, and Khoo. The group had varying opinions and felt that the balance of effects varies as it depended on the circulating variant and vaccination status of the patients and the attendant risk of severe disease.
Resources required
The group felt that the costs were moderate to deliver this intervention as this is an oral pill and the total costs for a single course would amount to around 1400Rs.
Certainty of evidence of required resources
No studies reporting this were reviewed by the group but the clinicians in the group were aware of the cost and hence felt that there was high certainty of evidence for required resources to implement this intervention.
Cost effectiveness
The panel discussed and agreed that there was no research evidence that evaluated cost of Molnupiravir in an Indian context, when other oral options were available.
Equity
At this point in time this intervention would probably reduce equity if found suitable and efficacious in Indian settings as cost are low and there is no need for hospitalization
Acceptability
The group felt that this intervention is likely to have wide acceptance by all the relevant stakeholders (policy-makers, patients and clinicians) as it is an oral drug and can be administered easily. Since it is an oral drug, monitoring the adherence of the patients is important to achieve desired effect. The group discussed that this should only be considered as an alternative as other efficacious options exist and are available and accessible. It could be safely used in older patients as they are less likely to be affected by teratogenicity concerns, though less evidence for benefit exists in this subgroup.
Feasibility
This is a feasible intervention if found efficacious as it is of low cost and can easily be delivered in a short course of 5 days.
Molnupiravir is an alternate oral antiviral to be given within 5 days of symptom onset in mild to moderate COVID-19. As a relatively affordable oral drug, and one of few available for mild to moderate COVID-19, it should be reserved for those at high risk of progression to severe disease. However, due to its questionable efficacy it should be considered for treatment only when other options like Remdesivir or Nirmatrelvir/ritonavir are not available. Due to risk of teratogenicity and predisposition to malignancies, Molnupiravir should be avoided as far as possible to women of child bearing age (avoid in partners and spouses as well) or in children. Clinicians, hospitals and policymakers should consider how to put appropriate measures in place to ensure patient safety. Additionally, as Molnupiravir is a new drug, caution should be taken to follow patients up closely, at least clinically, to allow rarer or unknown adverse effects to be detected.
The working group examined subgroup analysis concerning severity and vaccination status. They noted a mild benefit in terms of the outcome 'hospitalization or death at day 28' among patients with mild to moderate COVID-19 with Molnupiravir. Additionally, they observed that data were accessible for unvaccinated individuals in two studies, showing a mild benefit regarding the same.
In terms of mortality, there was a significant benefit among patients with mild and moderate COVID-19. Furthermore, in the subgroup of vaccinated individuals, mortality was significantly lower in patients treated with Molnupiravir.
Molnupiravir is an antiviral with an advantage of being an oral drug and thus can result in misuse. The current evidence reveals a small benefit in mild disease in those who are unvaccinated and risk factors. At present the pooled data does not suggest significant short-term or long term adverse events. This recommendation against the use of Molnupiravir will be reviewed as and when, any new evidence emerges.
The MOVE-out study recruited unvaccinated patients prior to the emergence of Omicron variant. Further research is needed for
1. Assessing treatment efficacy/effectiveness in fully vaccinated patients with mild illness and risk factors for progression
2. Assessing genotoxicity in more in-vitro and in-vivo models
3. Assessing the impact of Molnupiravir on inducing viral mutations that may have phenotypic consequences especially in immunocompromised individuals
4. Assessing the in-vitro activity of Molnupiravir against the constantly emerging Omicron variants.
- World Health Organization. Therapeutics and COVID-19: Living guideline, 10 November 2023. World Health Organization, Geneva. 2023. Available from: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-therapeutics-2023.2.
- EIDD-2801 [Internet]. [cited 2022 Jan 13]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/145996610
- First oral antiviral for COVID-19, Lagevrio (molnupiravir), approved by MHRA [Internet]. GOV.UK. [cited 2022 Feb 7]. Available from: https://www.gov.uk/government/news/first-oral-antiviral-for-covid-19-lagevrio-molnupiravir-approved-by-mhra
- Commissioner O of the. Coronavirus (COVID-19) Update: FDA Authorizes Additional Oral Antiviral for Treatment of COVID-19 in Certain Adults [Internet]. FDA. FDA; 2021 [cited 2022 Feb 7]. Available from: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-additional-oral-antiviral-treatment-covid-19-certain
- Preliminary data indicate COVID-19 vaccines remain effective against severe disease and hospitalisation caused by the Omicron variant [Internet]. European Medicines Agency. 2022 [cited 2022 Feb 7]. Available from: https://www.ema.europa.eu/en/news/preliminary-data-indicate-covid-19-vaccines-remain-effective-against-severe-disease-hospitalisation
- Molnupiravir and Drug Development at Emory | Emory University | Atlanta GA [Internet]. [cited 2022 Jan 13]. Available from: https://news.emory.edu/tags/topic/molnupiravir/index.html
- Fischer W, Eron JJ, Holman W, Cohen MS, Fang L, Szewczyk LJ, et al. Molnupiravir, an Oral Antiviral Treatment for COVID-19 [Internet]. 2021 Jun [cited 2022 Jan 15] p. 2021.06.17.21258639. Available from: https://www.medrxiv.org/content/10.1101/2021.06.17.21258639v1
- Bernal AJ, Silva MMG da, Musungaie DB, Kovalchuk E, Gonzalez A, Reyes VD, et al. Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients. New England Journal of Medicine [Internet]. 2021 Dec 16 [cited 2022 Jan 15]; Available from: https://www.nejm.org/doi/10.1056/NEJMoa2116044
- Khoo SH, Fitzgerald R, Fletcher T, Ewings S, Jaki T, Lyon R, et al. Optimal dose and safety of molnupiravir in patients with early SARS-CoV-2: a Phase I, open-label, dose-escalating, randomized controlled study. Journal of Antimicrobial Chemotherapy. 2021 Dec 1;76(12):3286–95.
- Zhou S, Hill CS, Sarkar S, Tse LV, Woodburn BMD, Schinazi RF, Sheahan TP, Baric RS, Heise MT, Swanstrom R. β-d-N4-hydroxycytidine Inhibits SARS-CoV-2 Through Lethal Mutagenesis But Is Also Mutagenic To Mammalian Cells. J Infect Dis. 2021 Aug 2;224(3):415-419. doi: 10.1093/infdis/jiab247. PMID: 33961695; PMCID: PMC8136050
- Khoo SH, FitzGerald R, Saunders G, Middleton C, Ahmad S, Edwards CJ, et al. Molnupiravir versus placebo in unvaccinated and vaccinated patients with early SARS-CoV-2 infection in the UK (AGILE CST-2): a randomised, placebo-controlled, double-blind, phase 2 trial. The Lancet Infectious Diseases. 2023 Feb;23(2):183–95.
- Tippabhotla SK, Lahiri DrS, D RR, Kandi C, V NP. Efficacy and Safety of Molnupiravir for the Treatment of Non-Hospitalized Adults With Mild COVID-19: A Randomized, Open-Label, Parallel-Group Phase 3 Trial. SSRN Journal [Internet]. 2022 [cited 2023 Dec 11]; Available from: https://www.ssrn.com/abstract=4042673
- Arribas JR, Bhagani S, Lobo SM, Khaertynova I, Mateu L, Fishchuk R, et al. Randomized Trial of Molnupiravir or Placebo in Patients Hospitalized with Covid-19. NEJM Evidence [Internet]. 2022 Jan 25 [cited 2023 Dec 11];1(2). Available from: https://evidence.nejm.org/doi/10.1056/EVIDoa2100044
- Caraco Y, Crofoot GE, Moncada PA, Galustyan AN, Musungaie DB, Payne B, et al. Phase 2/3 Trial of Molnupiravir for Treatment of Covid-19 in Nonhospitalized Adults. NEJM Evidence [Internet]. 2022 Jan 25 [cited 2023 Dec 11];1(2). Available from: https://evidence.nejm.org/doi/10.1056/EVIDoa2100043
- Butler C, Hobbs FDR, Gbinigie O, Rahman NM, Hayward G, Richards D, et al. Molnupiravir Plus Usual Care Versus Usual Care Alone as Early Treatment for Adults with COVID-19 at Increased Risk of Adverse Outcomes (PANORAMIC): Preliminary Analysis from the United Kingdom Randomised, Controlled Open-Label, Platform Adaptive Trial. SSRN Journal [Internet]. 2022 [cited 2023 Dec 11]; Available from: https://www.ssrn.com/abstract=4237902
Covid Management Guidelines India Group - Anti-viral Working Group. Molnupiravir. Covid Guidelines India; Published online on April 04, 2023; URL: Molnupiravir: Updated Recommendation – Covid Guidelines India (indiacovidguidelines.org)
