Prone positioning, or proning, is an inexpensive non-pharmacological intervention which is postulated to improve oxygenation by recruiting alveoli that are better perfused and hence decrease the ventilation- perfusion mismatch in COVID-19 pneumonia with acute respiratory distress syndrome (ARDS).
In ventilated patients with COVID-19 ARDS, the guidelines group decided to strongly recommend proning, as there is unambiguous evidence of this intervention in decreasing mortality in patients with non-COVID-19 ARDS who require invasive ventilation. The assumption underpinning this recommendation is that COVID-19 ARDS is not significantly different from non-COVID-19 ARDS.
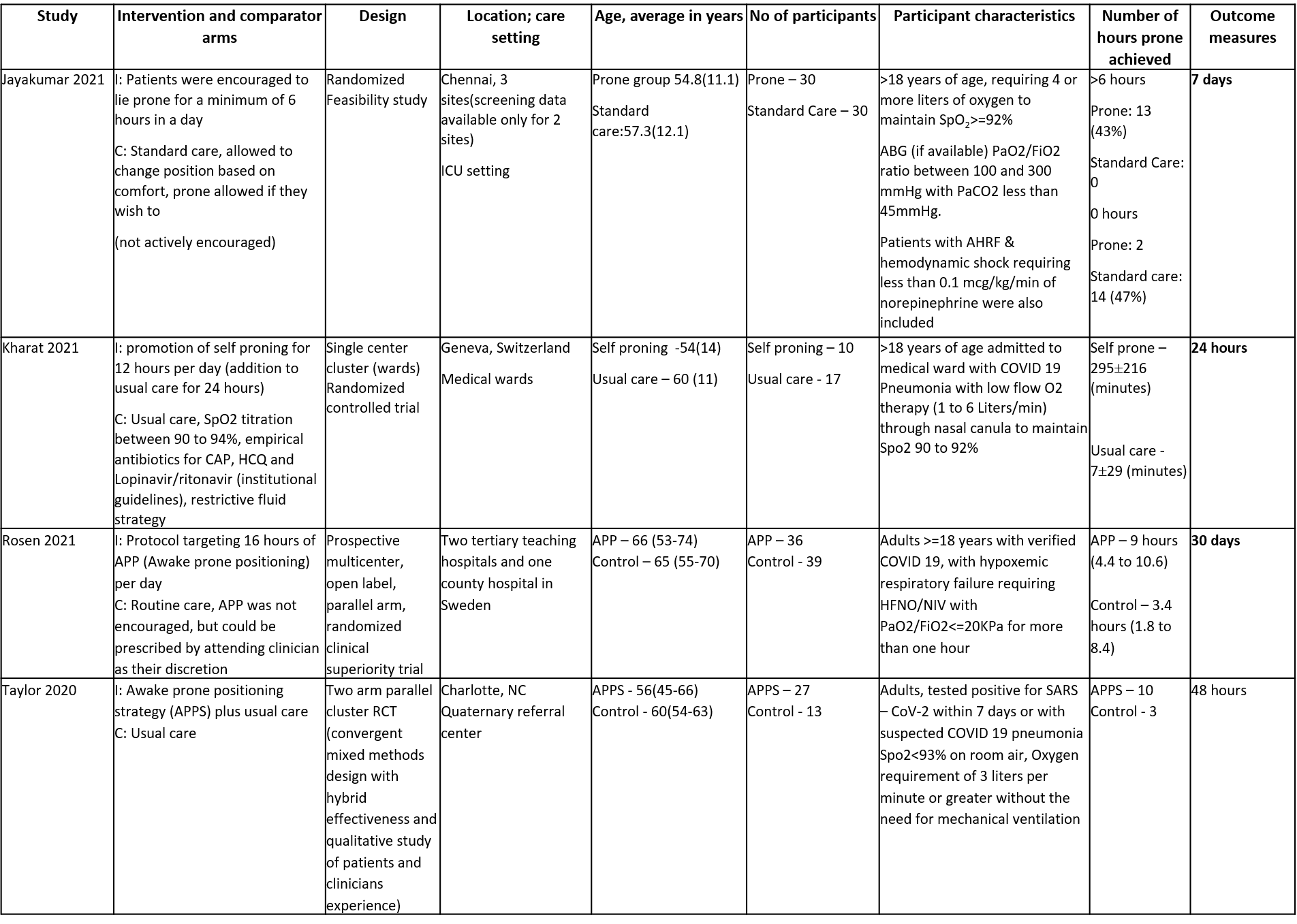
There have been 4 randomized controlled trials recruiting patients with moderate to severe COVID-19 studying awake self-positioning or proning against standard of care without prone positioning. The studies were marked by substantial heterogeneity, particularly in the duration of prone positioning. Compliance with the intervention was also of concern; all trials reported that the intended duration of prone positioning was not achieved. Hence, we decided not to pool these studies in a meta-analysis.
Due to the paucity of randomized trial evidence, observational cohorts reporting outcomes of interest were analyzed. There were 6 studies in non-intubated hypoxemic patients with COVID-19 included in our evidence summary. A meta-analysis of these revealed that awake proning /self-prone positioning improves oxygenation in the short term, as measured by PaO2, SpO2, PaO2/FiO2 ratio and SpO2/FiO2 ratio. The number of hours of self-prone positioning per day varied substantially between studies.
This led to only a conditional recommendation of awake proning /self-prone positioning in moderate and severe COVID-19, and in those with critical COVID-19 not receiving invasive mechanical ventilation, and a strong recommendation for proning in patients on invasive mechanical ventilation in critical COVID-19.
Date of latest search: 17th July 2021.
Date of completion & presentation to Expert Working Group: 19th July 2021.
Date of planned update: 17th January 2022
Evidence synthesis team: Lenny Vasanthan T, Deva Jedidiah, Richard Kirubakaran, Priscilla Rupali and Bhagteshwar Singh
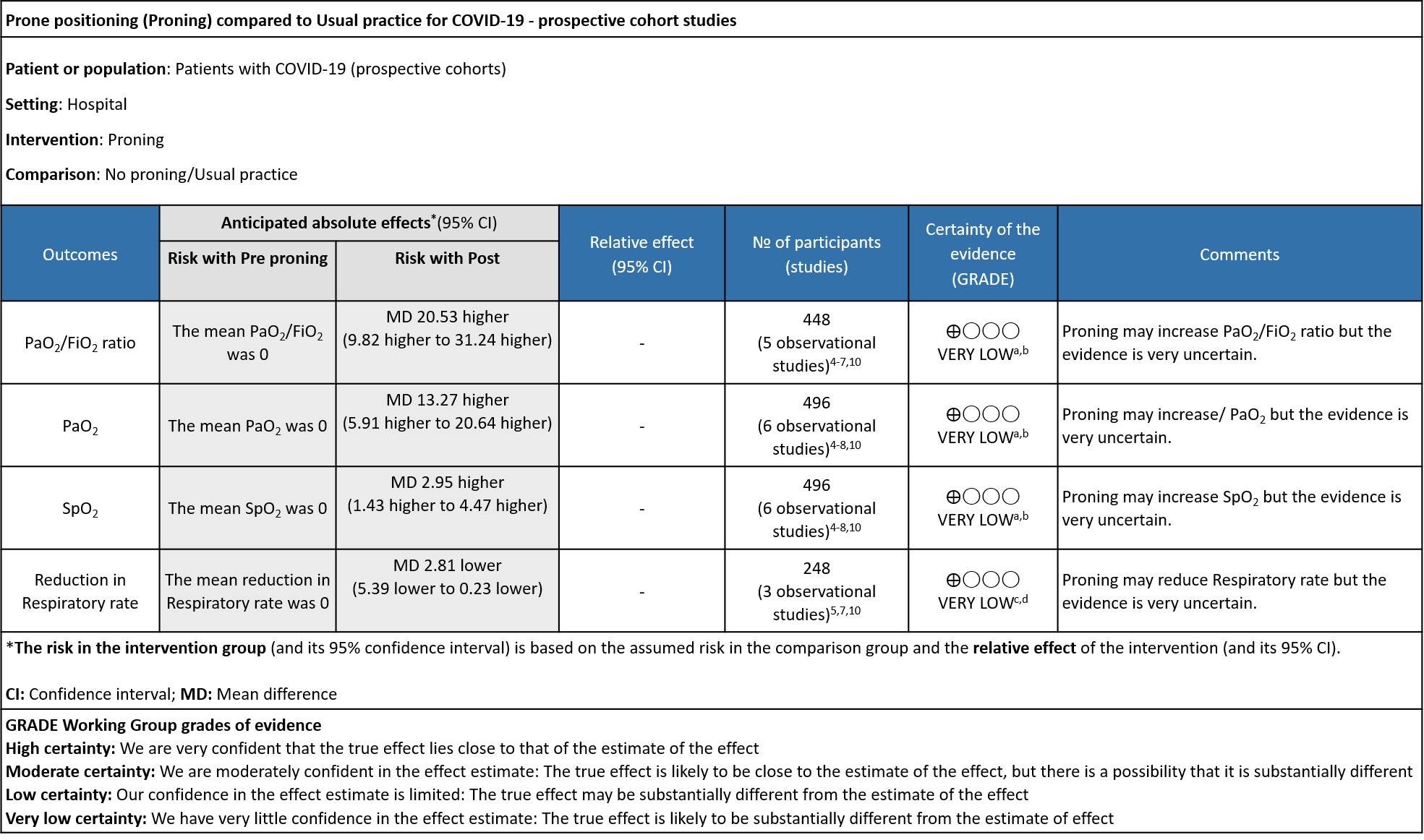
Explanations:
a. Downgraded by one level for serious Risk of Bias, Taboada and Ferrando had no non exposure group
b. Downgraded by two levels, I2 above 90%
c. Downgraded by one level for serious Risk of Bias, Ferrando had no non exposure group
d. Downgraded by two levels, I2 above 80%
Prone positioning (PP; also called proning) is a non-pharmacological modality used in the treatment of acute respiratory distress syndrome (ARDS). Prone positioning has been used in rehabilitation since early 1974 (Bryan 1974)1. Awake prone positioning is believed to recruit more lung tissue in those with mild hypoxia in moderate or severe COVID-19 by improving ventilation, and keeps alveolar units open, making breathing easier. Some regimens employ full-prone positioning alone, whereas others include a half-prone position, and lying laterally. All of these can be used sequentially in a cyclical manner throughout the day or during an episode of repositioning.
In severe ARDS, and in those on invasive mechanical ventilation, the major PROSEVA trial demonstrated a mortality benefit, with 16% mortality in the prone group vs 32.8% in the supine group (p=0.001)2. During the current COVID-19 pandemic, this modality has gained popularity due to evidence of improving oxygenation in persons with COVID-19 and thus decreasing need for oxygen therapy.
The second wave of the pandemic led to a severe and acute shortage of ICU beds. Home care had to be used for some patients who required oxygen therapy and it was incumbent upon health care workers to innovate to find ways to improve oxygenation with a lack of oxygen supply. Thus, awake prone positioning became popular at this time as it anecdotally helped individuals who had borderline hypoxia to be supported through natural recovery without requiring admission to hospital. Soon it was also recommended by the Ministry of Health and Family Welfare in individuals with COVID-19 whether at home or in hospital.3 However, there is clinical equipoise for use of proning in individuals with moderate to severe COVID-19.
PICO Question: Does prone positioning (half/lateral/full) improve oxygenation and reduce mortality in patients with symptomatic COVID-19?
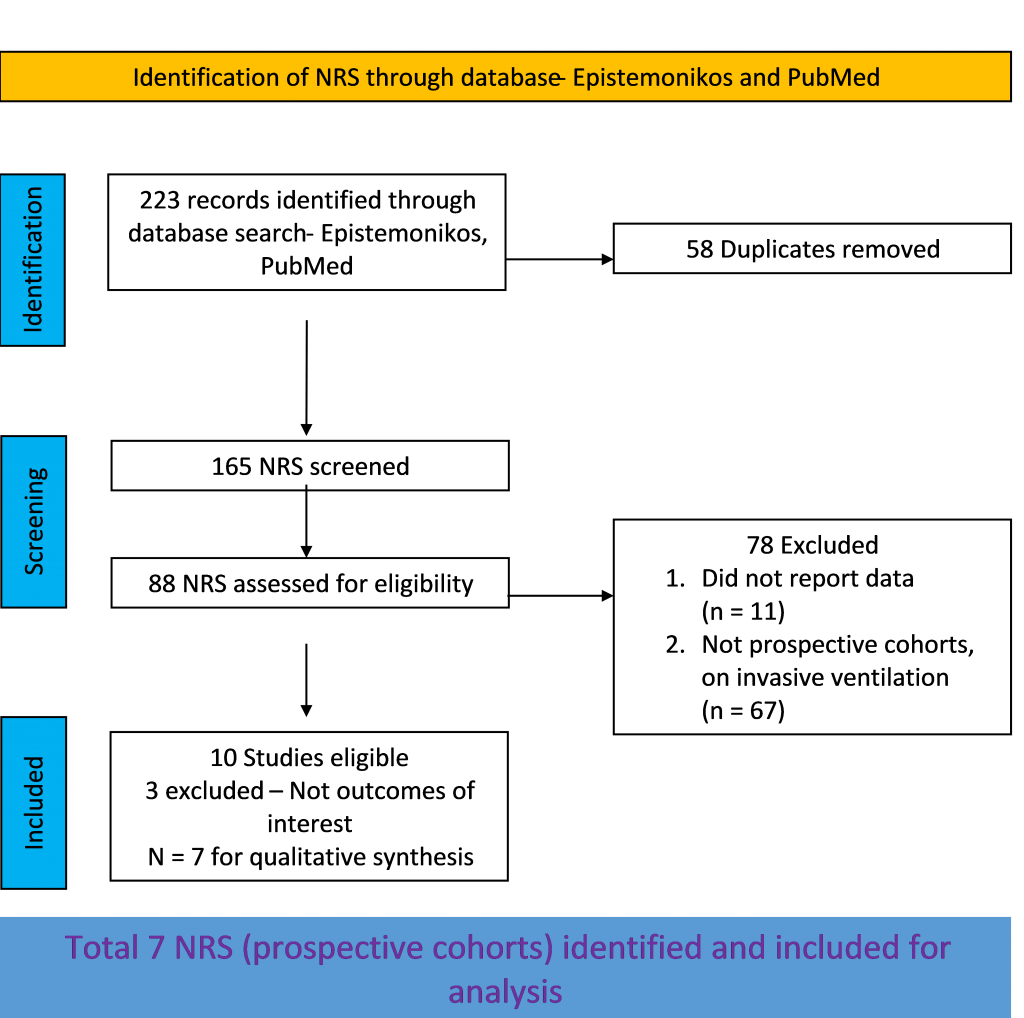
We searched PubMed, Epistemonikos, and the COVID‐19‐specific resource www.covid‐nma.com, for randomized controlled trials (RCTs) and cohort studies of any publication status and in any language. We also reviewed reference lists of systematic reviews and included studies. We performed all searches up to 17th July 2021.
Population: Patients in hospital with symptomatic COVID-19 of moderate, severe and critical severity with resting oxygen saturation <94% breathing room air.
Intervention: Prone positioning, self-awake proning
Control: Standard of care/placebo
Outcomes:
Primary:
Change in:
- Oxygenation/ventilatory setting
- Work of breathing
Progression to:
- Oxygen therapy
- Ventilation: non-invasive or invasive
- Critical or intensive care (any reason)
- Organ support
Secondary:
- Time to clinical improvement (WHO)
- Duration of ventilator support in hospital
- Duration of vasopressor support
- Mortality (all-cause) – at 28-30 days, or in-hospital
- Length of ICU stay
Adverse events: All and serious (including reduced chest wall compliance, change in pressure, obstruction/dislodgement, edema, increased need of sedatives, pressure sore)
Two reviewers independently screened search results using the online Rayyan tool. Data extraction was performed by one reviewer, and checked by another, using a piloted data extraction tool in Microsoft Word. Risk of bias (RoB) was assessed using the Cochrane RoB v2.0 tool (for the RCTs). The Newcastle Ottawa Scale (NOS) was used for the prospective cohorts. RoB was assessed by one reviewer and checked by a second reviewer.
For RCTs alone, the judgement was compared with the COVID-NMA judgement. If there was a difference in more than one domain in prospective cohorts or non-randomized studies (NRS) it was assessed by a third independent reviewer and a group consensus was obtained. We planned to use risk ratios (RR) for dichotomous outcomes and mean differences (MD) for continuous outcomes, with 95% confidence intervals (CIs); meta-analysis was performed using Review Manager (RevMan) v5.4. We used GRADE methodology to make summary of findings tables on GRADEPro GDT.
Our search found 4 RCTs and 13 cohort studies (7 prospective; 6 retrospective) after removing duplicates and excluding studies that did not match our PICO question. The four RCTs were not subjected to a meta-analysis because of heterogeneity in study duration (one study – 30 days, one study –7 days, 48 hours, 24 hours)intervention duration, and study design (convergent mixed methods design and cluster-randomized study design) being used. The team decided not to pool data from the very heterogeneously conducted and reported retrospective cohort studies. Out of the seven prospective cohort studies initially included, six prospective cohort studies were included for the meta-analysis; one study was excluded as it did not report our outcome of interest.
Randomized control trials:
There were four identified RCTs with 202 participants, who received awake prone positioning or self proning as part of their treatment, compared to usual care or standard care. The trials were conducted in the following countries - India, Switzerland, Sweden and USA. All studies were done in a hospital setting. All persons in the trial were provided supplemental oxygen if their saturation levels were below 92 to 94% on room air. (Refer ‘Summary of included studies’ for further details)
We included 6 studies (prospective cohorts) recruiting 496 participants, all of whom were adults, and all participants underwent prone positioning as an intervention [4-10]. There was one study each from Spain, China, USA, Italy, France, and UK. One study had participants from Spain and Andorra. All participants were admitted to a hospital, six of the seven studies were single-center studies and one was a multicenter study. All of the studies had participants who had the ability to self-prone in the hospital, the severity of illness was moderate to severe (5 studies), mild to moderate (1 study). In all six trials, the patients were on supplementary oxygen. The ‘Summary of characteristics of included studies’ table provides further details.
The risk of bias was assessed using the Newcastle Ottawa scale for all included studies. Four studies (Caputo6, Coppo7, Fazzini9, Zang5) was assessed as good quality, two studies (Elharrar8, Ferrando10) were deemed to be of fair quality and one study (Taboada4) was of poor quality.
We compared the following outcomes in the trials: change in PaO2/FiO2 ratio, PaO2 and SpO2; and reduction in respiratory rate. The outcomes were measured before and after prone positioning in the hospital. (See Summary of characteristics of included studies).
No comparative data could be extracted for the other outcome measures.
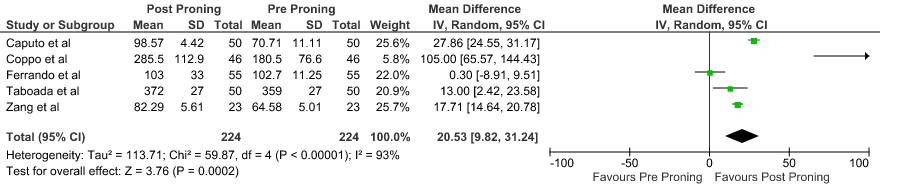
PaO2/FiO2 ratio: Pooled data from 5 Prospective cohort studies4-7,10 that included 448 hospital in-patients with COVID-19 indicated that the evidence is very uncertain with regard to the effect of proning on improving PaO2/FiO2ratio. The mean difference was 20.53 higher compared to baseline (95% CI 9.82 higher to 31.24 higher).
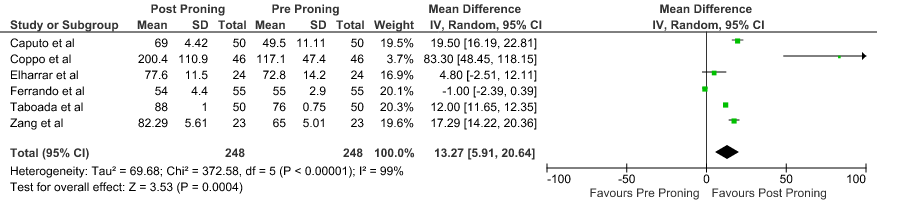
PaO2: Pooled data from 6 Prospective cohort studies4-8,10 that included 496 hospital in-patients with COVID-19 indicates that the evidence is very uncertain about the effect of proning on improving PaO2. The mean difference was 13.27 mmHg higher compared to baseline (95% CI 5.91 higher to 20.64 higher).
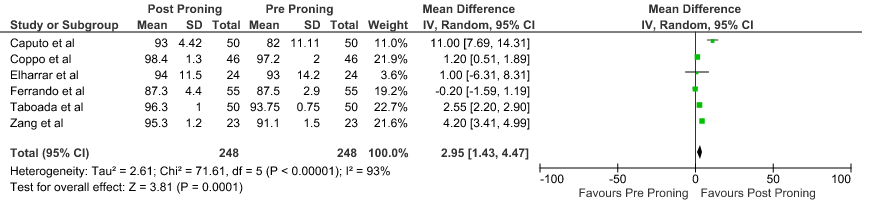
SpO2: Pooled data from 6 Prospective cohort studies4-8,10 that included 496 hospital in-patients with COVID-19 indicates that the evidence is very uncertain about the effect of proning on improving SpO2. The mean difference was 2.95% higher compared to baseline (95% CI 1.43 higher to 4.47 higher).
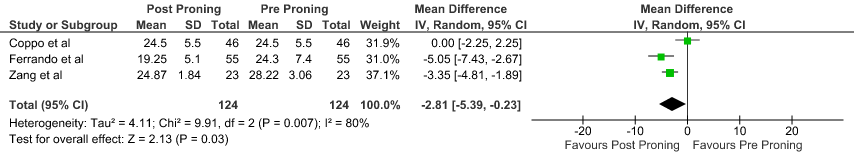
Reduction in respiratory rate: Pooled data from 3 Prospective cohort studies5,7,10 that included 496 hospital inpatients with COVID-19 indicates that the evidence is very uncertain about the effect of proning on reducing respiratory rate. The mean reduction in Respiratory rate 2.81 breaths per minute was lower compared to baseline (95% CI 5.39 lower to 0.23 lower).
Randomized control trials: 11-14
Prospective Cohort studies:4-10
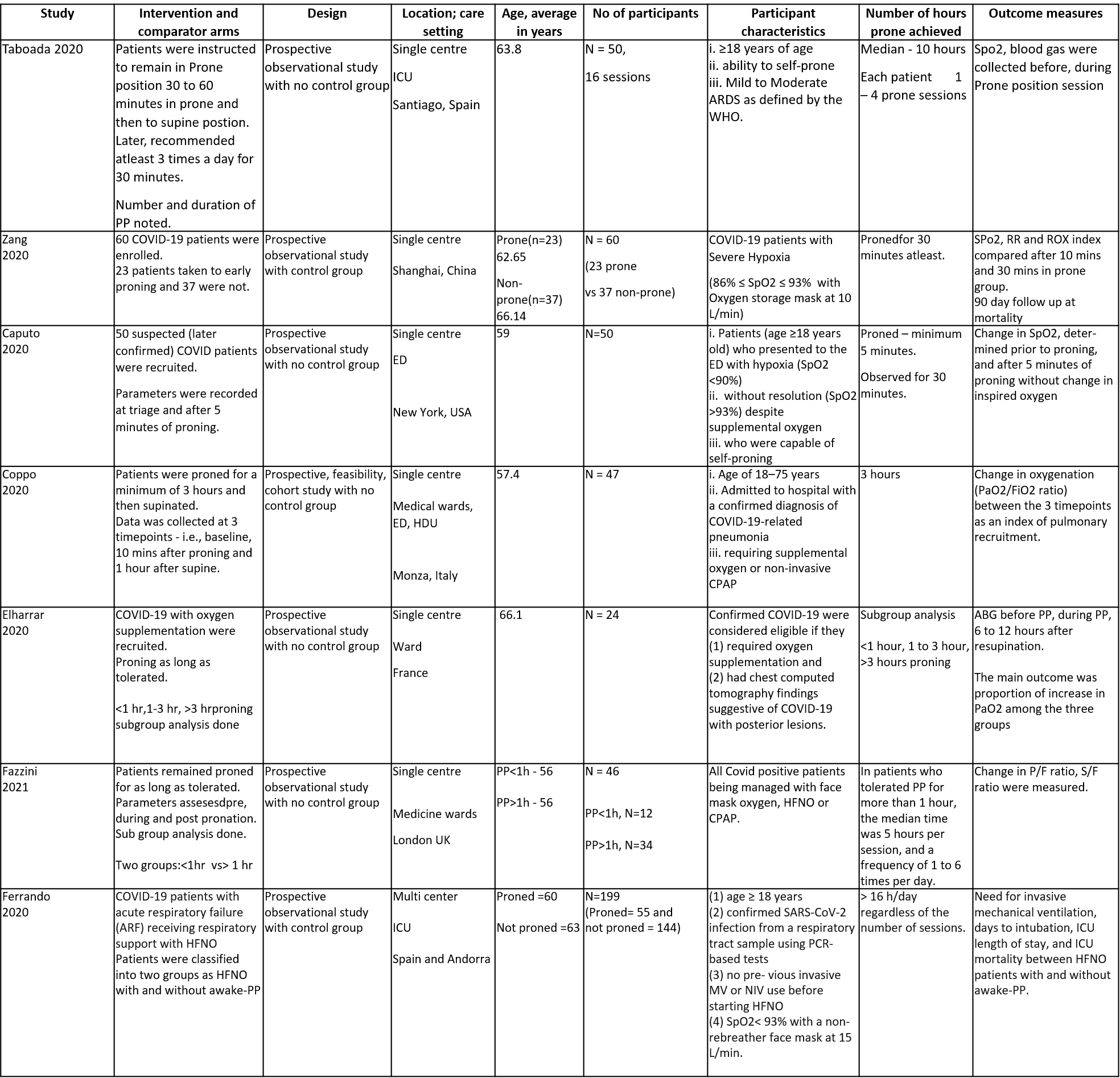
SpO2: pulse oxygen saturation, RR: respiratory rate, ROX index [ROX index=SpO2/(FiO2*RR)], PP: prone position, HFNC: high flow nasal cannula, NIV: non-invasive ventilation, IMV: invasive mechanical ventilation
ED - Emergency Department, HDU - High dependency unit, ICU - intensive care unit
P/F ratio - ratio of arterial oxygen partial pressure to fraction of inspired oxygen
S/F ratio - ratio of the peripheral capillary oxygen saturation to fraction of inspired oxygen
Prospective Cohorts:
1. Difference in PaO2/ FiO2 ratio before and after proning
2. Difference in PaO2 before and after proning
3. Difference in SpO2 before and after proning
4. Reduction in Respiratory rate before and after proning
The Respiratory Therapy and Other Supportive Therapy Group met on 19th July 2021 to consider Prone Positioning as a treatment for COVID-19. A further focused meeting with critical care physicians in the group took place on 5th August 2021, discussing prone positioning in severe to critical COVID-19, which was followed up by email discussions achieving consensus among group members. Conflict of interest declarations were reviewed by the Steering Committee; none were found to be relevant to prone positioning.
A summary and then more detailed explanations of the Expert Working Group's (EWG) judgements follow.
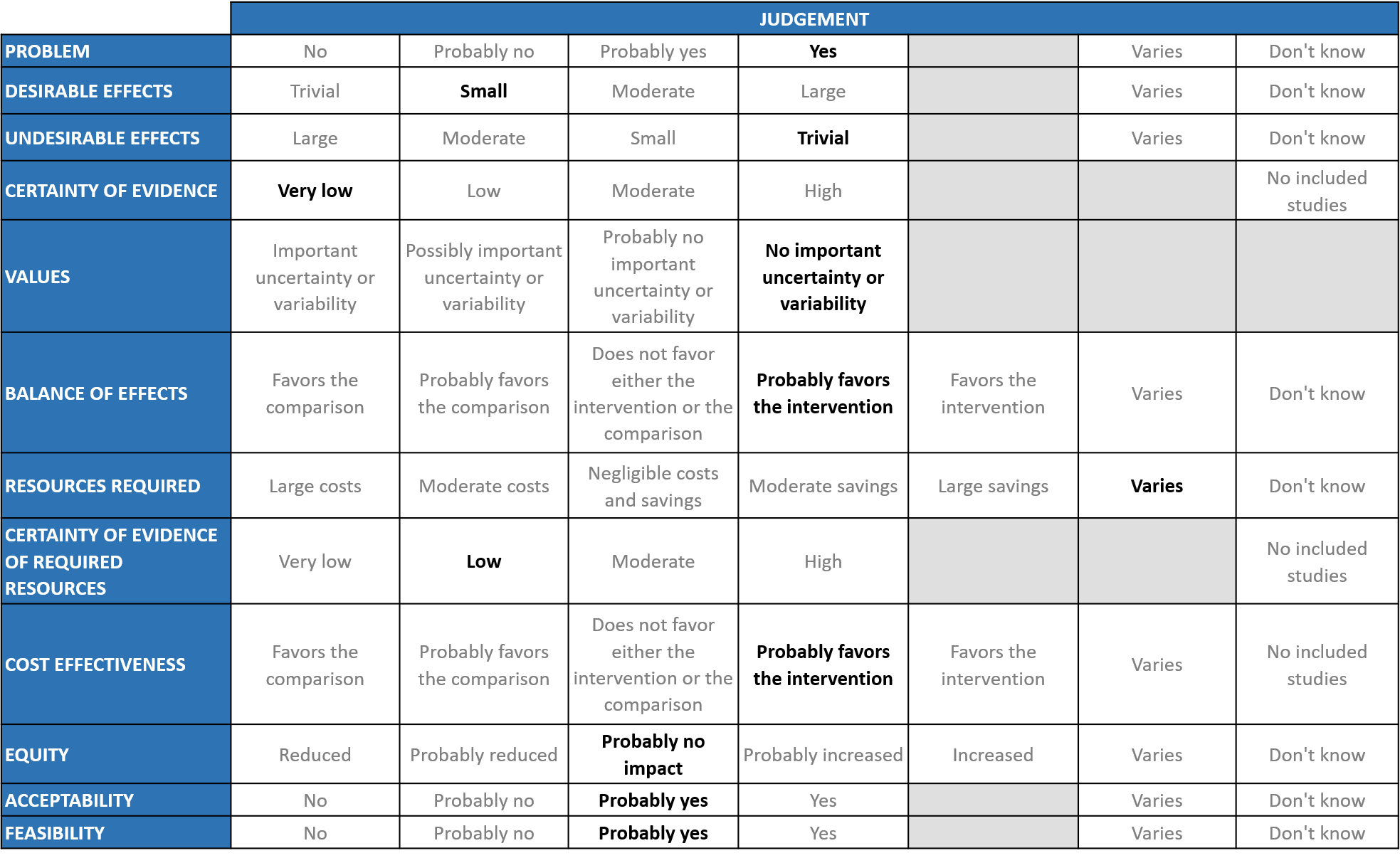
Problem
The COVID-19 pandemic in India with more than 30 million cases and over 0.39 million deaths has significantly impacted and stressed the health structure of the country. With a shortage of intensive care unit beds, oxygen and trained personnel the country is facing a major health crisis. The group judged the problem to be of utmost priority.
Desirable effects
The panel agreed that the evidence is lacking to suggest that proning has a clinically significant effect on all-cause mortality, progression to NIV /high flow nasal canula. Progression to IMV and also need for ICU was not signficant. Studies suggest that proning may have a clinically significant effect on PaO2/FiO2, Pao2, SpO2 and reduction in respiratory rate, though the evidence was graded as very uncertain. The expert working group (EWG) also noted potential improvement in oxygenation and based on RCTs 11-14, though these data were not pooled. Proning in critically ill patients with ARDS does not have equipoise. It is known to have a mortality benefit. Discussion was held and it was felt that we need to look at evidence in critical COVID-19 requiring intubation. However, intensivists were of the view that proning as a modality to improving oxygenation in severe ARDS is known. Hence the panel concluded that proning has a small desirable effect.
Undesirable effects
The data from some RCTs suggested that the adverse events like bedsore and dislodging of IV lines were less common in the groups with prone positioning in the RCTs, though it was unclear how valid it would be to conclude this based on small, heterogeneous trials. Anecdotally mild hypotension has been observed by some working group members who have provided the intervention (based on unpublished evidence, personal clinical experience). However, the EWG concluded that the undesirable effects of proning were thought to be trivial.
Certainty of evidence
Using GRADE methodology, the evidence synthesis team rated certainty of evidence as very low for all the outcomes.
Values
The EWG felt that there is no important uncertainty or variability on how people would value the main outcomes.
Balance of effects
The expert working group felt that the balance of effects probably favours the intervention. The group discussed at length about desirable effects about improvement in oxygenation, reduced escalation of care. Accidental disconnections and dislodging of tubes are apparently common in the ward, even though the opposite was suggested by some RCTs. But where feasible it is a good intervention to implement, with mitigation measures in place for potential undesirable effects.
Resources required
The resources required would include trained manpower (however existing staff could be redeployed), material resources, and a hospital facility capable of managing patients with ARDS. Proning schedules may be difficult to implement unless they are made part of routine care and led by a specific supervising lead. Proning may decrease oxygen requirements and hence may bring down capital costs as well. Intensive care units have 1:1 staffing but this is not the same in other wards and hence additional resources required vary according to the setting. The costs of these resources would also vary depending on the setting. The group includes clinicians in different types of Indian hospitals who have a good idea of drug and hospitalization costs.
Certainty of evidence of required resources
No studies reporting this were reviewed by the group but the clinicians in the group were aware of the difficulties in generalizing costs, as mentioned above, and hence felt that there was low certainty of evidence for required resources to implement this intervention.
Cost effectiveness
The group discussed that even though there was no research evidence that evaluated cost in an Indian context, it probably favors the intervention, as this intervention was of clinical benefit and would not be high relative to others. The group felt that despite the additional manpower that may or may not be needed, this is an intervention that should be implemented wherever possible choosing the right kind of setting and patient population.
Equity
The intervention itself is cheap and probably will have no impact on equity although appropriate implementation may require an appropriate setting and in some cases adequate personnel.
Acceptability
The group felt that this intervention is likely to have wide acceptance by all the relevant stakeholders (policy-makers, patients and clinicians), even though it is uncomfortable and hence patients might be initially reluctant, but this would be overcome if patient were motivated based on the improvement in their clinical status.
Feasibility
This is a feasible intervention but mechanisms need to be put in place for proning protocols.
The working group discussions concluded that awake prone positioning was a reasonably feasible intervention for patients with moderate and severe COVID-19 disease. The practical challenges include patient related factors such as degree of respiratory distress (it may be difficult or unsafe to have a patient with severe distress to maintain an awake prone positioning), patient habitus (it may be difficult in obese individuals), level of co-operation. Often mild sedation, anxiolysis and/or analgesics may be required to facilitate prone positioning. The duration of awake prone management that leads to best outcomes is unknown. Even though there is no strong evidence to show benefit in overall outcome, due to the physiological effects on oxygenation and ventilation, it is plausible that awake prone ventilation when combined with Non-Invasive ventilation or high-flow oxygen therapy, could be an effective form of respiratory support that may reduce oxygen requirements, reduce the need for invasive ventilation, ICU care or death. System related factors such as nurse-patient ratios, availability of allied health practitioners or physiotherapists, location of patients (ICU vs wards) may determine the ease with which awake prone ventilation may be carried out.
With regard to prone ventilation in invasively ventilated patients, prone ventilation for COVID-19 patients with Moderate to Severe ARDS may have a mortality benefit (especially if PaO2/FiO2 ratios are 60% and when carried out for at least 16 hours) as with other forms of ARDS. This reflects best practice in units where staff are familiar with this process.
Contraindications to prone ventilation include raised intracranial pressure, increased intrabdominal pressure, vertebral injuries or instability, severe haemodynamic instability. Common complications include dislodgement of tubes (Endotracheal or Nasogastric), excessive discharge of oral and gastric secretions, facial and tongue oedema, eye injuries, pressure related injuries to dependent areas. Patients must be frequently monitored for these, while in prone position.
No subgroup analysis was performed by individual studies or in the meta-analysis.
Considered decisions have to be made based on individual patient’s condition and response to prone positioning, resources and experience of clinicians attending to the patient.
No specific recommendations can be made regarding the following subgroups of interest based on available evidence:
- Pre-existing chronic lung disease
- Obesity
- Co-existing cardiac failure (acute/chronic)
- Age > 65 years
- Spine or chest wall deformities
- Pre-existing neurological disease with deficits
- Pregnancy
Prone positioning in hospitalized moderate to non-intubated critical patients is a low risk and low-cost intervention with small benefits in improving oxygenation and preventing escalation of care. The side effects related to the practice are minimal, however there is lack of well-defined protocols for the practice. While further studies are warranted and as the data emerge, the group will monitor and evaluate the clinical relevance, benefits and the best set protocols for the awake self-prone positioning.
There is considerable heterogeneity in implementation of the intervention in various studies precluding a clear cut answer to its efficacy, however since it is a low cost, feasible intervention it is being practiced everywhere. However, the group felt that the following could be considered:
- RCT comparing full-prone position and semi-prone positions in awake patients with COVID-19 and early ARDS, measuring the effect on mortality and requirement of invasive mechanical ventilation.
- Studies comparing the effect of prone position in mechanically ventilated patients with COVID-19 with severe ARDS vs. in patients with ARDS of other infectious etiologies.
- Bryan C (1974). Comments of a Devil’s Advocate. American Review of Respiratory Disease, 110(6P2), pp. 143–144
- Claude Guérin C et al., (2013)Prone positioning in severe acute respiratory distress syndrome. (PROSEVA trial). N Engl J Med. 2013 Jun 6;368(23):2159-68. doi: 10.1056/NEJMoa1214103. Epub 2013 May 20.
- Ministry of Health and family welfare. https://www.mohfw.gov.in/pdf/COVID19ProningforSelfcare3.pdf accessed on June 8,2021
- Taboada M et al (2020). Short-term outcomes of 50 patients with acute respiratory distress by COVID-19 where prone positioning was used outside the ICU. J Clin Anesth. 2020 Dec;67:110028. doi: 10.1016/j.jclinane.2020.110028. Epub 2020 Aug 18.
- Zang et al (2020). Efficacy of early prone position for COVID-19 patients with severe hypoxia: a single-center prospective cohort study. Intensive Care Med. 2020 Oct;46(10):1927-1929. doi: 10.1007/s00134-020-06182-4. Epub 2020 Jul 22.
- Caputo et al (2020). Early Self-Proning in Awake, Non-intubated Patients in the Emergency Department: A Single ED's Experience During the COVID-19 Pandemic. Acad Emerg Med. 2020 May;27(5):375-378. doi: 10.1111/acem.13994.
- Coppo et al (2020).Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020 Aug;8(8):765-774. doi: 10.1016/S2213-2600(20)30268-X. Epub 2020 Jun 19.
- Elharrar et al. (2020). Use of Prone Positioning in Nonintubated Patients With COVID-19 and Hypoxemic Acute Respiratory Failure. JAMA. 2020 Jun 9;323(22):2336-2338. doi: 10.1001/jama.2020.8255.
- Fazzini et al. (2020). Effectiveness of prone position in spontaneously breathing patients with COVID-19: A prospective cohort study.Journal of the Intensive Care Society. https://doi.org/10.1177/1751143721996542
- Ferrando et al. (2020). Awake prone positioning does not reduce the risk of intubation in COVID-19 treated with high-flow nasal oxygen therapy: a multicenter, adjusted cohort study. Crit Care. 2020 Oct 6;24(1):597. doi: 10.1186/s13054-020-03314-6.
- Jayakumar D et al (2021). Awake prone position in adult nonintubated patients with acute hypoxaemic respiratory failure secondary to COVID-19:A multi-centre feasibility randomized controlled trial.J Intensive Care Med. 2021 May 5:8850666211014480 (online)
- Kharat et al.,Self proning in COVID-19 patients on low flow oxygen therapy: A cluster randomised controlled trial. ERJ Open Res 2021 Mar 8;7(1):00692-2020.
- Rosen J, Research Square, 2021. Awake Prone Positioning in Patients with Hypoxemic Respiratory Failure Due to COVID-19: The PROFLO Multicenter Randomized Clinical Trial.
- Taylor SP et al (2020) Awake-prone positioning strategy for non-intubated hypoxic patients with COVID -19: A pilot trial with embedded implementation evaluation. Ann Am Thorac Soc. 2020 Dec 23.
Covid Management Guidelines India Group - Other Supportive Management Working Group. Prone Positioning. Covid Guidelines India; Published online on November 05th, 2021; URL: https://indiacovidguidelines.org/prone-positioning/ (accessed ).