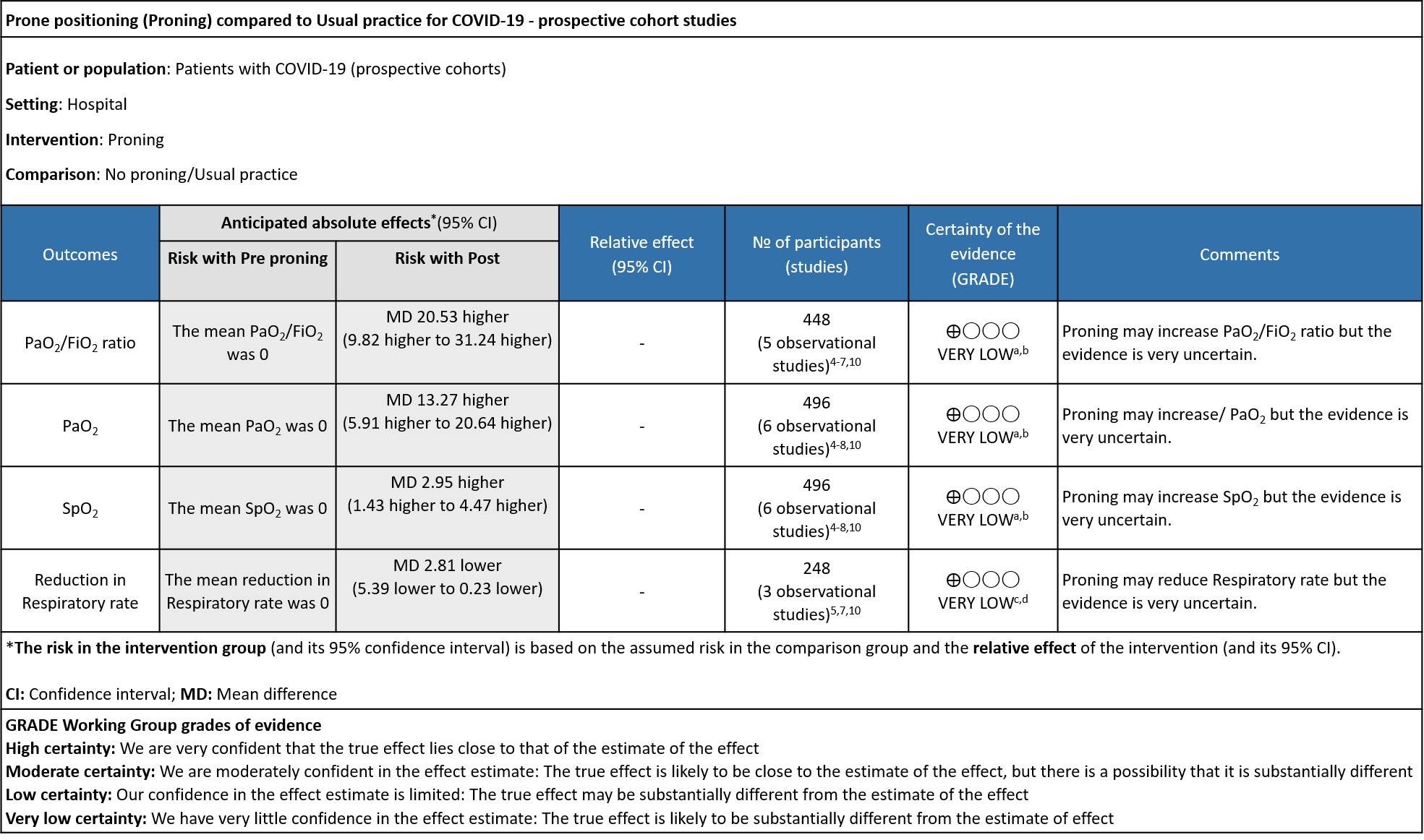
Explanations:
a. Downgraded by one level for serious Risk of Bias, Taboada and Ferrando had no non exposure group
b. Downgraded by two levels, I2 above 90%
c. Downgraded by one level for serious Risk of Bias, Ferrando had no non exposure group
d. Downgraded by two levels, I2 above 80%
Prone positioning (PP; also called proning) is a non-pharmacological modality used in the treatment of acute respiratory distress syndrome (ARDS). Prone positioning has been used in rehabilitation since early 1974 (Bryan 1974)1. Awake prone positioning is believed to recruit more lung tissue in those with mild hypoxia in moderate or severe COVID-19 by improving ventilation, and keeps alveolar units open, making breathing easier. Some regimens employ full-prone positioning alone, whereas others include a half-prone position, and lying laterally. All of these can be used sequentially in a cyclical manner throughout the day or during an episode of repositioning.
In severe ARDS, and in those on invasive mechanical ventilation, the major PROSEVA trial demonstrated a mortality benefit, with 16% mortality in the prone group vs 32.8% in the supine group (p=0.001)2. During the current COVID-19 pandemic, this modality has gained popularity due to evidence of improving oxygenation in persons with COVID-19 and thus decreasing need for oxygen therapy.
The second wave of the pandemic led to a severe and acute shortage of ICU beds. Home care had to be used for some patients who required oxygen therapy and it was incumbent upon health care workers to innovate to find ways to improve oxygenation with a lack of oxygen supply. Thus, awake prone positioning became popular at this time as it anecdotally helped individuals who had borderline hypoxia to be supported through natural recovery without requiring admission to hospital. Soon it was also recommended by the Ministry of Health and Family Welfare in individuals with COVID-19 whether at home or in hospital.3 However, there is clinical equipoise for use of proning in individuals with moderate to severe COVID-19.
PICO Question: Does prone positioning (half/lateral/full) improve oxygenation and reduce mortality in patients with symptomatic COVID-19?
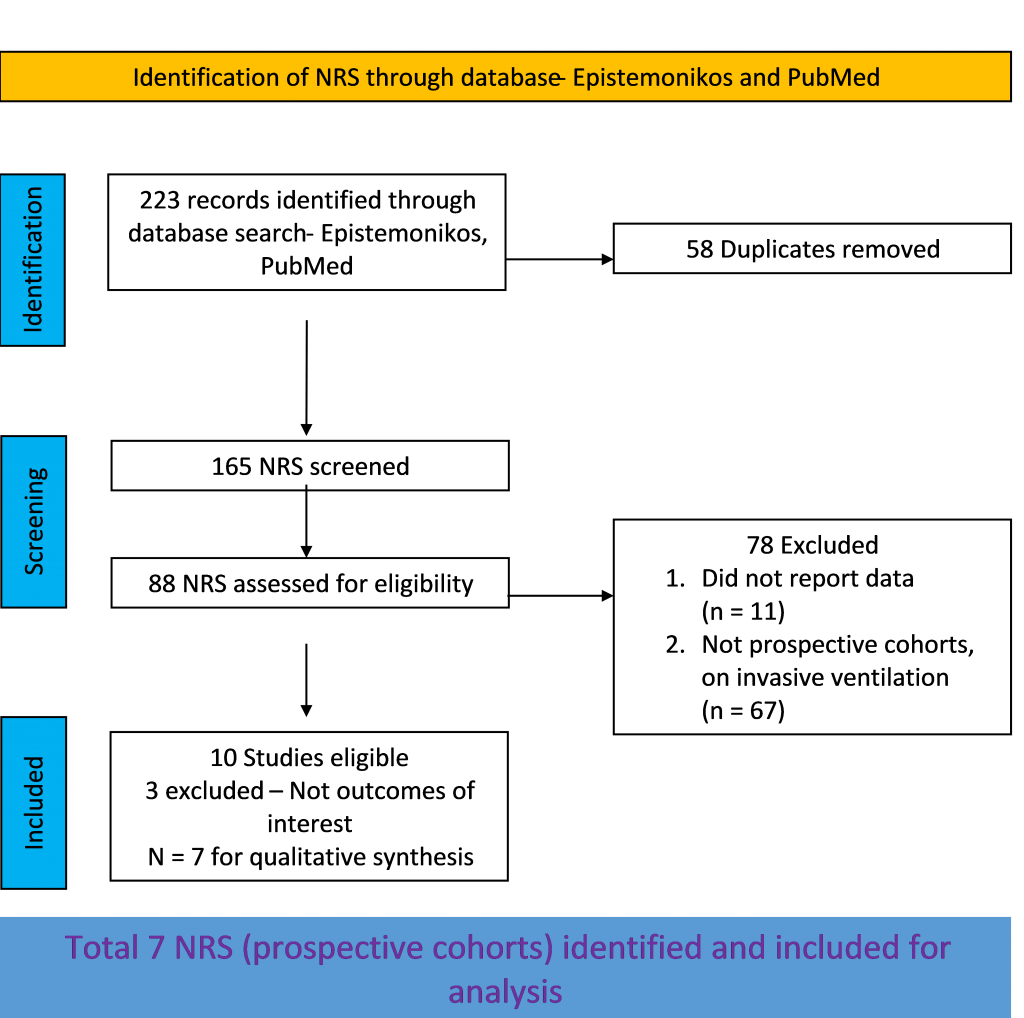
We searched PubMed, Epistemonikos, and the COVID‐19‐specific resource www.covid‐nma.com, for randomized controlled trials (RCTs) and cohort studies of any publication status and in any language. We also reviewed reference lists of systematic reviews and included studies. We performed all searches up to 17th July 2021.
Population: Patients in hospital with symptomatic COVID-19 of moderate, severe and critical severity with resting oxygen saturation <94% breathing room air.
Intervention: Prone positioning, self-awake proning
Control: Standard of care/placebo
Outcomes:
Primary:
Change in:
- Oxygenation/ventilatory setting
- Work of breathing
Progression to:
- Oxygen therapy
- Ventilation: non-invasive or invasive
- Critical or intensive care (any reason)
- Organ support
Secondary:
- Time to clinical improvement (WHO)
- Duration of ventilator support in hospital
- Duration of vasopressor support
- Mortality (all-cause) – at 28-30 days, or in-hospital
- Length of ICU stay
Adverse events: All and serious (including reduced chest wall compliance, change in pressure, obstruction/dislodgement, edema, increased need of sedatives, pressure sore)
Two reviewers independently screened search results using the online Rayyan tool. Data extraction was performed by one reviewer, and checked by another, using a piloted data extraction tool in Microsoft Word. Risk of bias (RoB) was assessed using the Cochrane RoB v2.0 tool (for the RCTs). The Newcastle Ottawa Scale (NOS) was used for the prospective cohorts. RoB was assessed by one reviewer and checked by a second reviewer.
For RCTs alone, the judgement was compared with the COVID-NMA judgement. If there was a difference in more than one domain in prospective cohorts or non-randomized studies (NRS) it was assessed by a third independent reviewer and a group consensus was obtained. We planned to use risk ratios (RR) for dichotomous outcomes and mean differences (MD) for continuous outcomes, with 95% confidence intervals (CIs); meta-analysis was performed using Review Manager (RevMan) v5.4. We used GRADE methodology to make summary of findings tables on GRADEPro GDT.
Our search found 4 RCTs and 13 cohort studies (7 prospective; 6 retrospective) after removing duplicates and excluding studies that did not match our PICO question. The four RCTs were not subjected to a meta-analysis because of heterogeneity in study duration (one study – 30 days, one study –7 days, 48 hours, 24 hours)intervention duration, and study design (convergent mixed methods design and cluster-randomized study design) being used. The team decided not to pool data from the very heterogeneously conducted and reported retrospective cohort studies. Out of the seven prospective cohort studies initially included, six prospective cohort studies were included for the meta-analysis; one study was excluded as it did not report our outcome of interest.
Randomized control trials:
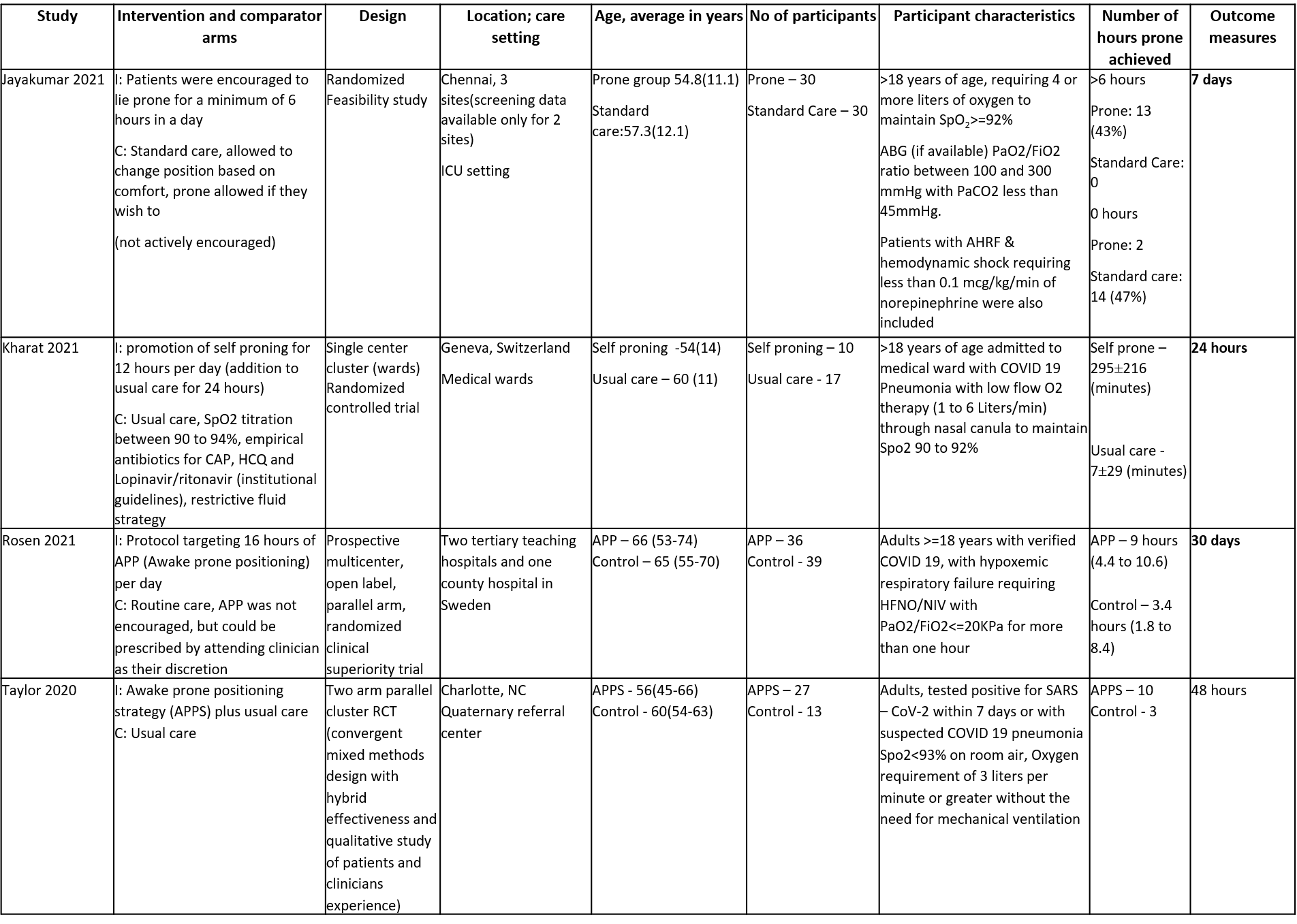
There were four identified RCTs with 202 participants, who received awake prone positioning or self proning as part of their treatment, compared to usual care or standard care. The trials were conducted in the following countries - India, Switzerland, Sweden and USA. All studies were done in a hospital setting. All persons in the trial were provided supplemental oxygen if their saturation levels were below 92 to 94% on room air. (Refer ‘Summary of included studies’ for further details)
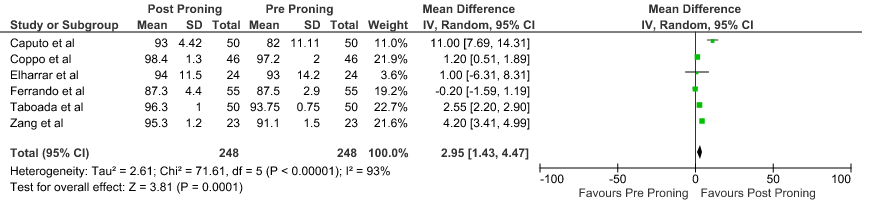
We included 6 studies (prospective cohorts) recruiting 496 participants, all of whom were adults, and all participants underwent prone positioning as an intervention [4-10]. There was one study each from Spain, China, USA, Italy, France, and UK. One study had participants from Spain and Andorra. All participants were admitted to a hospital, six of the seven studies were single-center studies and one was a multicenter study. All of the studies had participants who had the ability to self-prone in the hospital, the severity of illness was moderate to severe (5 studies), mild to moderate (1 study). In all six trials, the patients were on supplementary oxygen. The ‘Summary of characteristics of included studies’ table provides further details.
The risk of bias was assessed using the Newcastle Ottawa scale for all included studies. Four studies (Caputo6, Coppo7, Fazzini9, Zang5) was assessed as good quality, two studies (Elharrar8, Ferrando10) were deemed to be of fair quality and one study (Taboada4) was of poor quality.
We compared the following outcomes in the trials: change in PaO2/FiO2 ratio, PaO2 and SpO2; and reduction in respiratory rate. The outcomes were measured before and after prone positioning in the hospital. (See Summary of characteristics of included studies).
No comparative data could be extracted for the other outcome measures.
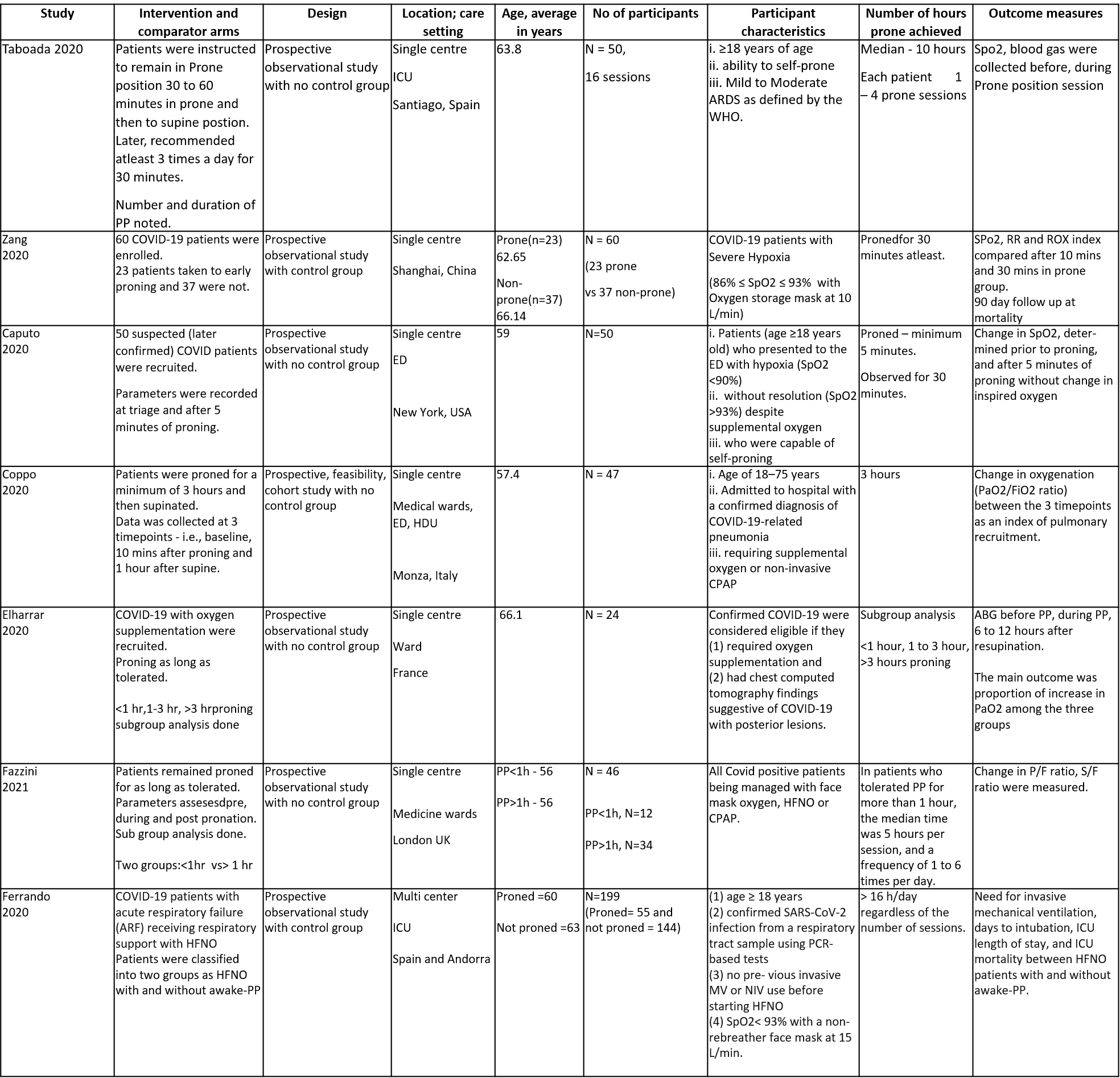
PaO2/FiO2 ratio: Pooled data from 5 Prospective cohort studies4-7,10 that included 448 hospital in-patients with COVID-19 indicated that the evidence is very uncertain with regard to the effect of proning on improving PaO2/FiO2ratio. The mean difference was 20.53 higher compared to baseline (95% CI 9.82 higher to 31.24 higher).
PaO2: Pooled data from 6 Prospective cohort studies4-8,10 that included 496 hospital in-patients with COVID-19 indicates that the evidence is very uncertain about the effect of proning on improving PaO2. The mean difference was 13.27 mmHg higher compared to baseline (95% CI 5.91 higher to 20.64 higher).
SpO2: Pooled data from 6 Prospective cohort studies4-8,10 that included 496 hospital in-patients with COVID-19 indicates that the evidence is very uncertain about the effect of proning on improving SpO2. The mean difference was 2.95% higher compared to baseline (95% CI 1.43 higher to 4.47 higher).
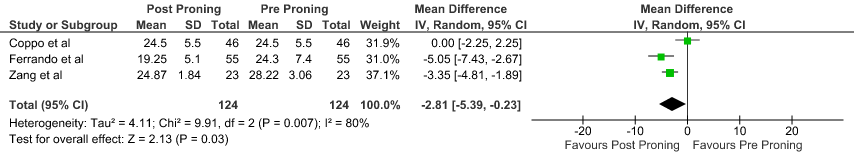
Reduction in respiratory rate: Pooled data from 3 Prospective cohort studies5,7,10 that included 496 hospital inpatients with COVID-19 indicates that the evidence is very uncertain about the effect of proning on reducing respiratory rate. The mean reduction in Respiratory rate 2.81 breaths per minute was lower compared to baseline (95% CI 5.39 lower to 0.23 lower).
Randomized control trials: 11-14
Prospective Cohort studies:4-10
SpO2: pulse oxygen saturation, RR: respiratory rate, ROX index [ROX index=SpO2/(FiO2*RR)], PP: prone position, HFNC: high flow nasal cannula, NIV: non-invasive ventilation, IMV: invasive mechanical ventilation
ED - Emergency Department, HDU - High dependency unit, ICU - intensive care unit
P/F ratio - ratio of arterial oxygen partial pressure to fraction of inspired oxygen
S/F ratio - ratio of the peripheral capillary oxygen saturation to fraction of inspired oxygen
Prospective Cohorts:
1. Difference in PaO2/ FiO2 ratio before and after proning
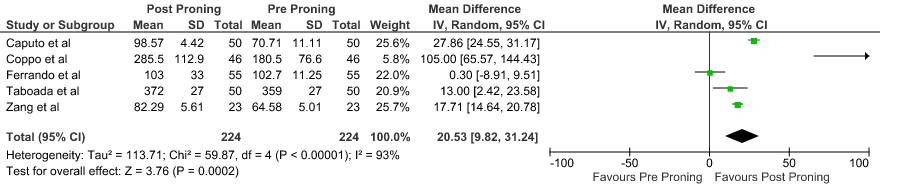
2. Difference in PaO2 before and after proning
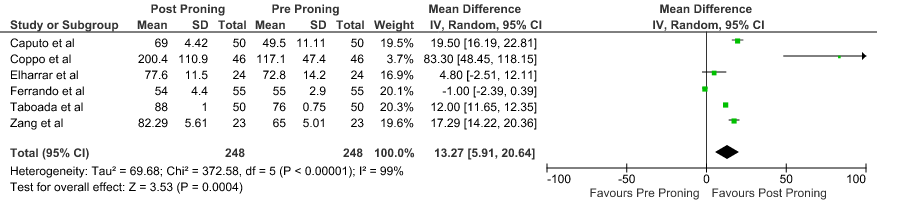
3. Difference in SpO2 before and after proning
4. Reduction in Respiratory rate before and after proning