Supplemental oxygen is the key intervention for severely and critically unwell COVID-19 patients. Oxygen is often administered liberally to acutely ill adults, but the evidence of benefit vs. risk of achieving high oxygen saturations in the blood is unclear, though in some conditions risk of harm has been demonstrated. The two essential questions that needed an answer were the SpO2 cut-off point for initiation of oxygen therapy and the ideal target range of SpO2 that should be maintained while on oxygen and other respiratory support therapy. If a patient can be successfully treated at lower targets without complications, unnecessary over-oxygenation and oxygen wastage could be minimised.
During the peak of the second wave of the SARS CoV-2 pandemic, India faced a severe oxygen shortage2-3. The government rapidly increased oxygen supply to various states4.
To preserve oxygen reserves and avoid wastage, various measures were looked at, such as:
- Timing of initiation of oxygen therapy,
- Target peripheral oxygen saturation (SpO2) range with the most clinical benefit,
- Lowest safe target oxygenation range,
- Timing of intubation and ventilation to achieve the lowest oxygen use
In COVID-19, World Health Organization (WHO) recommends that the target SpO2 should be ≥ 90%, and supplemental oxygen should be initiated below this cut-off. While an upper limit was not prescribed, it was understood that the patient should have a SpO2 of 90% or above at all times5. The US National Institutes of Health, British Thoracic Society, Italian Thoracic Society and the ICMR Covid-19 National Taskforce (India) recommend a SpO2 target of 92% to 96%6-8. This is based on the IOTA systematic review and LOCO2 randomized control trial, both based on non-COVID patients9,10. While the IOTA systematic review includes a high-quality meta-analysis, the population and interventions included in the analysis were diverse. In IOTA, substantial weight was given to trials that included patients with myocardial infarction, neurological disorders, trauma and surgery. Most studies included for analysis defined the interventions (conservative/lower SpO2 target vs liberal/higher SpO2 targets) based on a pre-fixed standard fraction of inhaled oxygen (FiO2) delivered to the patient, rather than titration of FiO2 to arrive at a target SpO2 range.
For studies on this topic, we searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Epistemonikos, and the COVID‐19‐specific resource covid19.recmap.org published up to 13th October 2021.
Our population, pre-defined by the Expert Working Group, was inpatients with confirmed or suspected COVID-19 with specific sub-populations: Pre-existing COPD, Obesity, Co-existing cardiac failure (acute/chronic) and Age >65 years.
The intervention was defined as active titration of oxygen delivery or respiratory support by measuring saturation at-least every 6 hours to target a SpO2 90-94%.
The comparison was defined as active titration of oxygen delivery or respiratory support by measuring saturation at-least every 6 hours to target a SpO2 95-100%.
We planned to extract data for the following outcomes, predefined by the Expert Working Group:
Primary outcome:
• All-cause Mortality
• Need for ventilation (IMV or NIV)
Secondary Outcomes:
• Time to clinical improvement (WHO ordinal scale or other definitions)
• Length of stay in hospital
• Duration of days free from invasive ventilation
• Length of stay in critical care
Adverse events:
1. All
2. Serious
3. Hypoxemia-related events:
-
-
- Mesenteric ischemia
- Myocardial infarction/ischemia
-
4. Others as specified by trials/reviews
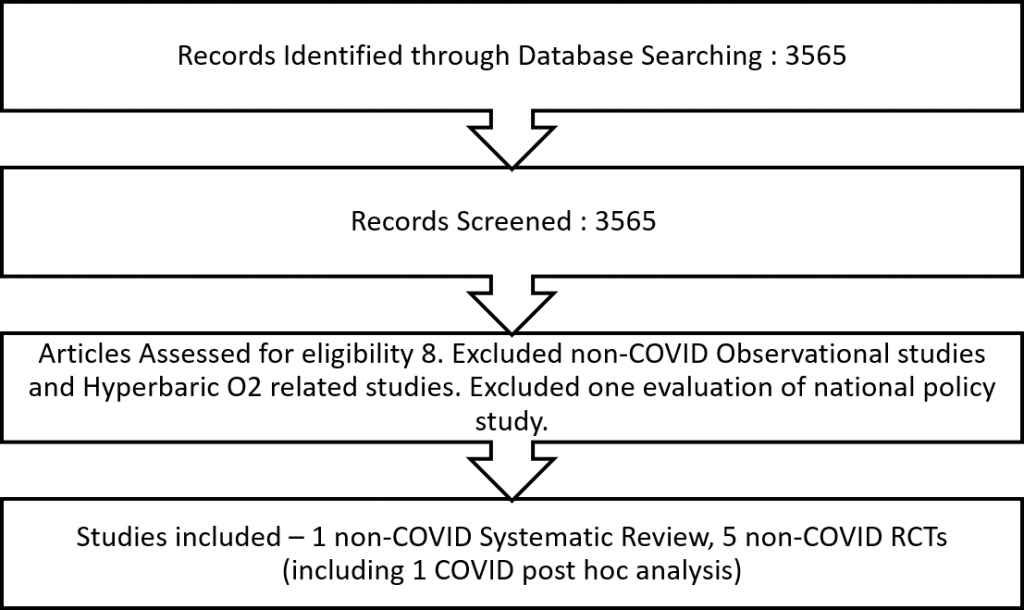
We found the non-COVID IOTA review, five non-COVID RCTs, with one of them performing a post-hoc subgroup analysis of COVID-19 patients.
Two reviewers independently assessed the eligibility of search results. Since all RCTs were non-COVID and the COVID subgroup analysis from the HOT-ICU trial13 was small and underpowered, we did not perform meta-analysis, and described the findings narratively.
Comments on the non-COVID RCTs.
• While all these were ICU based trials, only CLOSE 2016, LOCO2 and ICU ROX trials included mechanically ventilated patients at recruitment. OXYGEN ICU 2016 and the HOT ICU 2021 trials included patients in the ICU irrespective of their need for ventilation.
• The population varied across the trials. The OXYGEN ICU 2016 and CLOSE 2016 trials recruited only 35% of patients with medical causes of respiratory failure, and the rest had surgical causes. ICU ROX 2020 did not mention the nature of the underlying illness and instead provided details on where the patients were brought to ICU from, for example,the emergency ward and operation theatre. 57% of the HOT ICU 2021 trial patients had pneumonia, while the rest had non-pulmonary causes.
• Trials varied in their reporting of the syndrome necessitating oxygen supplementation, such as respiratory failure and acute respiratory distress syndrome (ARDS), and their causes. Most studies had recruited patients with type 1 respiratory failure; while some had ARDS, others were respiratory failure due to other causes. The following were the proportion of patients with documented ARDS in these trials: OXYGEN ICU 2016 (did not report), CLOSE 2016 (33 - 35%), ICU ROX 2020 (67 - 71%), HOT ICU 2021 (12 - 13%), LOCO2 2020 (100%); OXYGEN ICU 2016 (did not report)
• There was indirectness of evidence due to the differences in SpO2 targets in each arm across the various RCTs. None of the trials was close to our predefined definition of intervention (conservative;SpO2 90-94%) and comparison (liberal;95-100%).
• Some studies monitored partial pressure of oxygen from blood gas analysis while other studies used a peripheral SpO2 monitor and some used both. It is well known that cold peripheries, peripheral vascular compromise, abnormal haemoglobin, shock and vasoconstriction can cause differences in correlation between SpO2 and PaO2 at a particular point, which limits comparability between trials using SpO2 and those using PaO2.
• Implemented/resultant SpO2 varied from the target in some trials. However, as the “intervention” is a package of actions to achieve a target, the effect of this is unclear on the directness of the evidence.
• Monitoring of the patients to pick up deviations from the intended interventions was not uniform across studies. While the LOCO2 2020 trial used six-hourly blood gas analysis, HOT ICU 2021 performed blood gas analysis twice-daily.
HOT ICU COVID-19 subgroup analysis.
The HOT ICU 2021 trial was recruiting patients until the latter half of 2020. They had a subgroup of confirmed COVID-19 PCR-positive patients. The authors performed a posthoc analysis of the COVID positive subgroup and published it separately. There was no difference in mortality between the arms with conservative saturation target group (PaO2 60mmHg) compared to the liberal saturation (PaO2 90mmHg) target group. However, the conservative saturation target arm had a significantly lower percentage of life support-free days than the liberal arm. This significant difference was not present when the whole HOT ICU 2021 trial data (including the COVID-19 and non-COVID-19 participants) were analysed together. Here, life support was defined as the use of invasive or non-invasive mechanical ventilation, or continuous positive airway pressure, infusion of vasopressors or inotropic agents, or any form of renal replacement therapy.
HOT ICU post-hoc COVID subgroup analysis.
This subgroup had a sample size of around 100 and was not sufficiently powered to describe the outcomes meaningfully. The oxygenation target was primarily based on twice-daily monitoring of arterial partial pressure of oxygen. Intermittent SpO2 monitoring was done as per the discretion of the treating doctor to adjust the FiO2 to reach the target PaO2 levels. The twelve-hour gap in ABG monitoring could have delayed the adjustment needed in the deviated PaO2 to attain the target range.
• Mortality was around 41% in both arms and was generally higher than other RCTs, however this may be explained by the mortality risk of COVID-19 ARDS earlier in the pandemic. Also, the mortality described is only available for 90 days. Whereas clinically, a one-month mortality would be more useful
• Invasive mechanical ventilation: At recruitment, 44% of the conservative arm and 55% of the liberal arm were already intubated. Around 83% of conservative target arm patients and 97% of liberal target arm group required invasive mechanical ventilation by the end of the study.
• Requirement for intubation (new): 39% of the conservative arm and 41% of the liberal arm needed intubation for the first time after trial recruitment.
Summary:
We did not consider the IOTA systematic review in the evidence contributing directly to this recommendation as the population and definition of interventions were very different from that in our PICO.
The non-COVID RCTs also provided only indirect evidence. One safety concern with lower SpO2 targets emerged from one trial, with mesenteric ischaemia being more common in the group with the lower SpO2 target, though this target (88-92%) allowed lower SpO2 than that considered in our PICO (90-94%). The HOT ICU trial was a post hoc analysis with 109 patients and the data is not powered adequately to make meaningful recommendations.
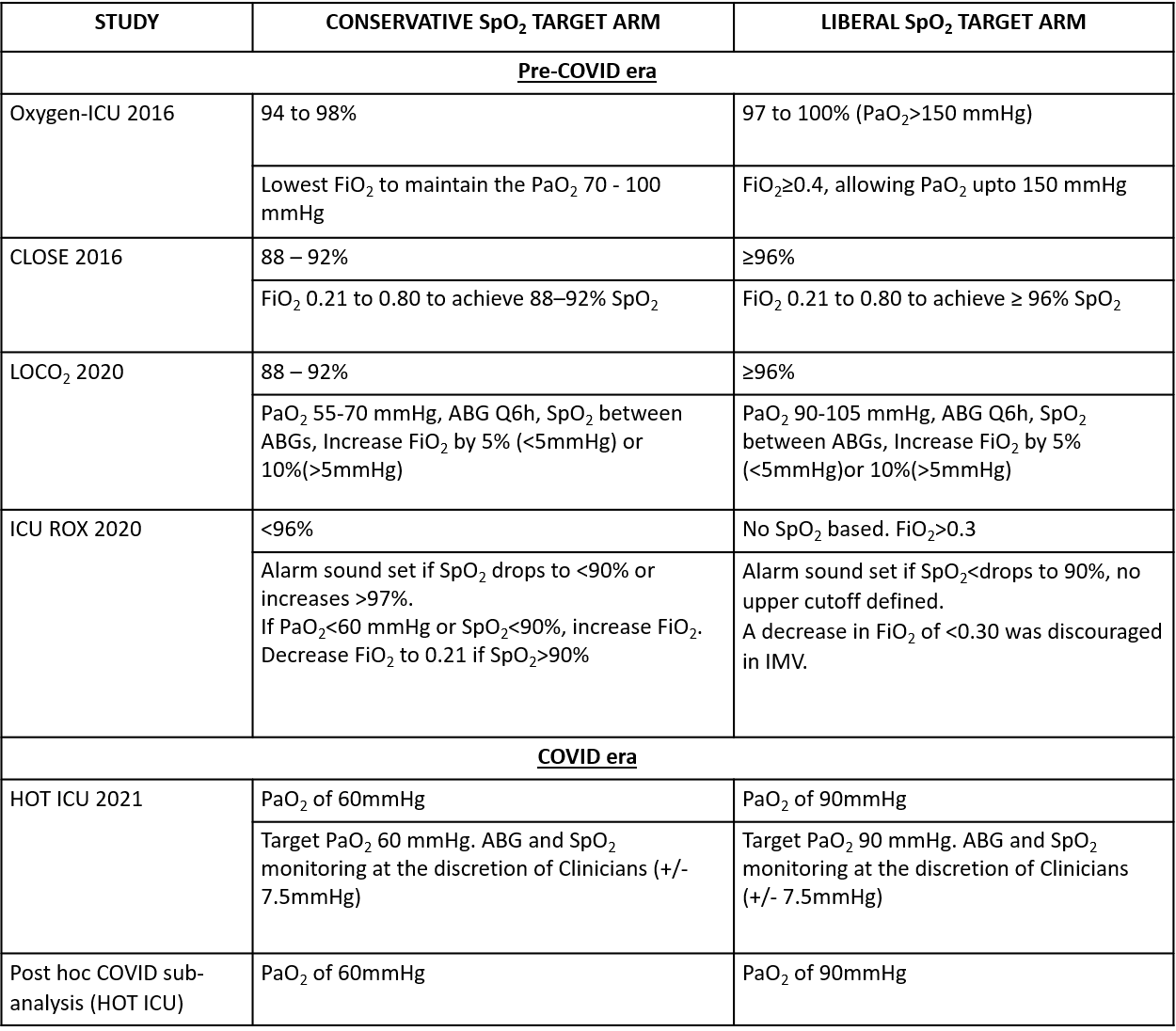
We critically looked at the five non-COVID RCTs and the post hoc subgroup analysis on COVID-19 patients. The definition of the conservative oxygen arm and the liberal oxygen arm was different across the studies (Table 2). The interventions to maintain the desired SpO2 target were also different for each arm and varied across the studies. Table 2 summarizes these essential differences.
1. Intensive care unit (ICU) Mortality
The Oxygen ICU Trial 2016 reported that patients in the arm with a conservative SpO2 target of 94-98% had lower ICU mortality compared to a more liberal target of 97% - 100% SpO2. The CLOSE 2016 trial and the LOCO2 trial also reported ICU mortality, which did not significantly differ between the two arms.
2. 90-day Mortality
The LOCO2 trial 2020 showed that a conservative SpO2 target of 88-92% had higher 90-day mortality than a liberal target of > 97%. CLOSE 2016, ICU ROX 2020 trial and Oxygen ICU 2021 also reported 90-day mortality, which did not significantly differ between the two arms.
3. Length of stay in hospital and ICU
Only OXYGEN ICU 2016 and CLOSE 2016 trials reported length of stay in hospital and length of stay in ICU. Both these outcomes were not significantly different between the two arms.
4. Invasive Mechanical Ventilation-free days
The CLOSE 2016 and the ICU ROX 2020 trials reported the number of invasive mechanical ventilation-free days. Neither trial reported a significant difference between the two arms.
5. Adverse Events
The LOCO2 trial 2020 was prematurely stopped due to mesenteric ischaemia in the conservative (lower) oxygen target arm; 5.1% (1.7%–11.4%) vs 0. The prevalence of arrhythmias, seizures and cerebrovascular events (reported to be stroke) were also higher in the conservative oxygen therapy arm. The HOT ICU 2021 trial also reported mesenteric ischaemia, arrhythmias, seizures and strokes, but they were not significantly different between the two arms.
Table 1: List of RCTs included in evidence synthesis.
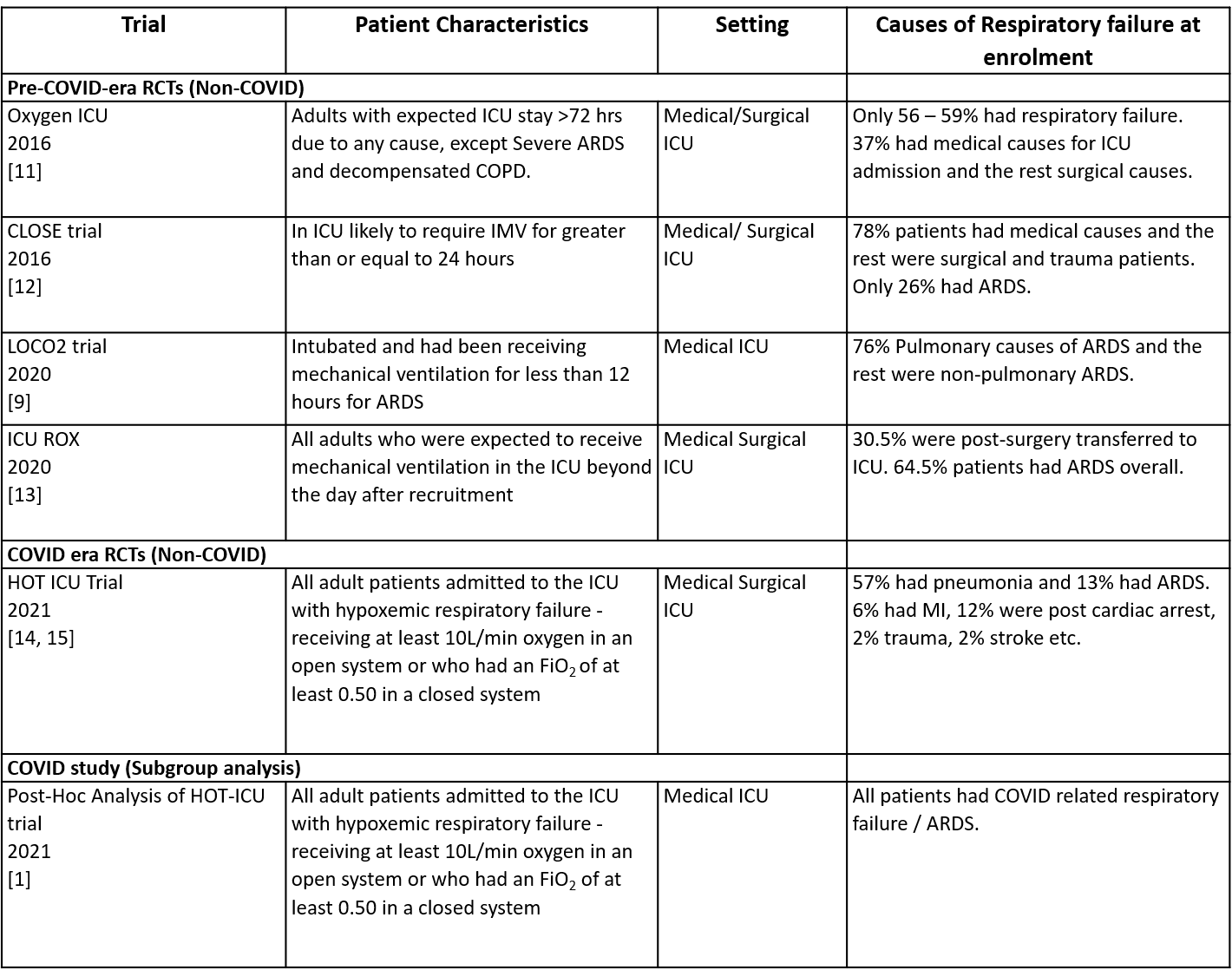
ARDS, acute respiratory distress syndrome; FiO2, fraction of inspired oxygen; ICU, intensive care unit; IMV, invasive mechanical ventilation.
Table 2: Summary of interventions and saturation targets of the RCTs.