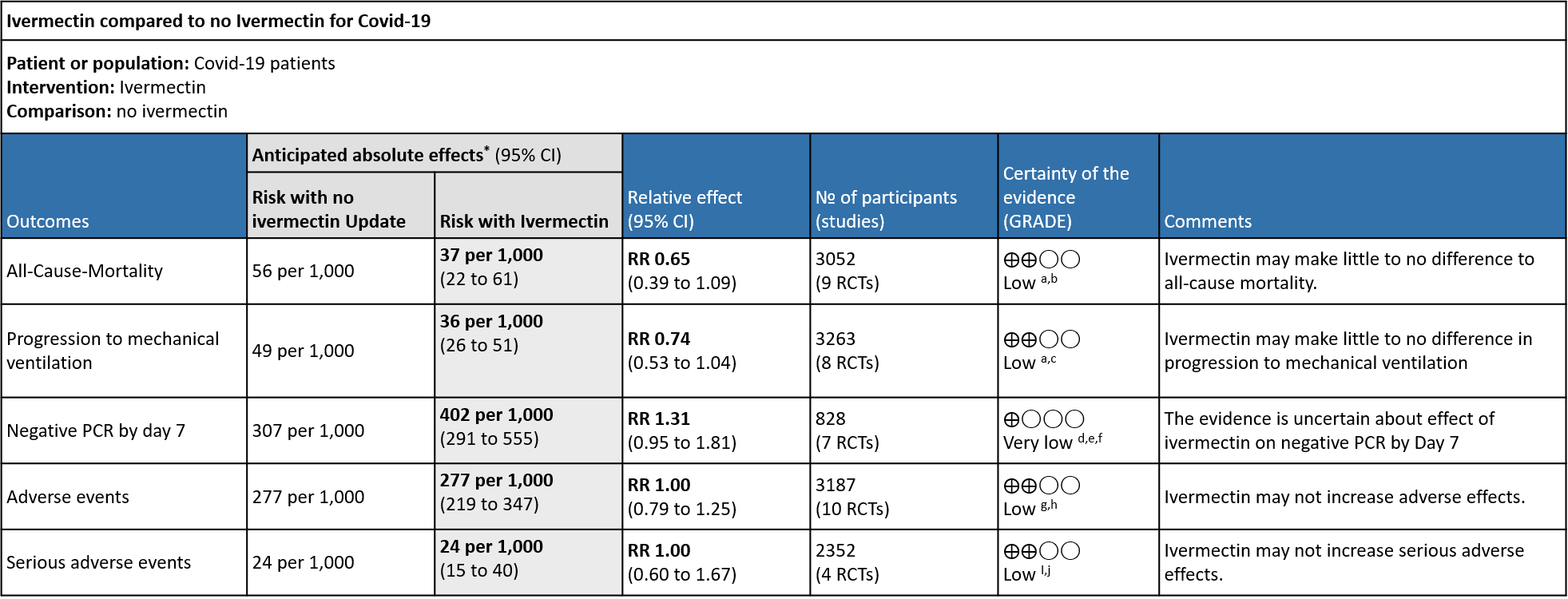
Explanations:
a. Downgraded by one level for serious imprecision, due to small absolute number of events, and CIs include important potential benefit and important potential harm.
b. Downgraded by one level for serious risk of bias. Due to Galan 2021 and Niaee 2021 having high risk of bias, and Gonzalez 2021 , Ravikirti 2021 , Abd Elsalam and Shahbaznejad 2021 having some concerns for risk of bias.
c. Downgraded by one level for serious risk of bias, due to Abd Elsalam , Galan 2021, Ravikirti 2021Shahbaznejad and I-tech trial having some concerns for risk of bias.
d. Downgraded by two levels for very serious risk of bias, due to Ahmed 2020 and Bukhari 2021 having high risk of bias and Bieber having some concerns for risk of bias for this outcome.
e. Downgraded by one level for serious inconsistency, due to substantial heterogeneity (I-squared=64%) and visually some trials having point effect estimates very far from those of other trials.
f. Downgraded by one level for serious imprecision, due to CIs overlapping no effect and inability to exclude important benefit.
g. Downgraded by one level for serious risk of bias., due to Chaccour 2021, Chachar 2021, Rocha et. al etc having high risk of bias (accounts for 15% weightage).
h. Downgraded by one level for serious imprecision, due to CIs overlapping including important potential benefit and important potential harm.
i. Downgraded by one level for serious risk of bias, due to Gonzalez 2021 having high risk of bias
j. Downgraded by one level for serious imprecision, due to CIs including important potential benefit and important potential harm.
Ivermectin has been shown to inhibit the replication of SARS CoV2 in vitro; it binds and destabilises the viral protein and prevents it from entering the nucleus (24). However, the drug dosages used in these laboratory studies far exceed those that have been used for other conditions (25). Drug doses and levels required to achieve therapeutic effects in COVID-19 infection in humans based on these studies may be safe, but this has not been studied in clinical trials (26). An additional potential effect may be in modulating the immune system, though this is yet to be studied thoroughly in humans (27).
Although Ivermectin is generally well tolerated, adverse effects like dizziness, tachycardia, postural hypotension, diarrhoea, arthralgia, facial and peripheral oedema have been reported even with single doses as used in parasitic diseases (28). Encephalopathy with permanent disability has been reported when ivermectin has been used in the treatment of onchocerciasis or other parasitic diseases (28). It is predominantly metabolized in the liver (CYP3A4), which may lead to drug-drug interactions.
Due to lack of conclusive evidence from trials, World Health Organization recommends use of ivermectin only in clinical trials (29). Use continues widely, including self-medication, especially in low- and middle-income countries due to easy availability and low cost of the drug (30). Multiple trials on Ivermectin on covid-19 were retracted due to questionable methodology and lack of reliable data. (21,22)
This review aims to provide a summary of the available evidence from randomised clinical trials of ivermectin for treatment of acute COVID-19, for any dose or duration, so the Expert Working Group can provide a recommendation to guide clinicians and researchers regarding the appropriate use of this drug.
We used Cochrane rapid review methods. We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Epistemonikos, and the COVID‐19‐specific resource www.covid‐nma.com, for studies of any publication status and in any language published from March 2020 up to 07th June 2022. We also reviewed reference lists of systematic reviews and included studies. We contacted researchers to identify unpublished and ongoing studies.
We included randomized controlled trials (RCTs) testing ivermectin treatment of any dose or duration in people with acute COVID‐19, whether suspected or confirmed. Trials were included if the intervention arm did not combine ivermectin with another experimental drug, and if the comparator arm did not include ivermectin (this could involve use of placebo, standard care, or other potentially active drugs). We excluded trials that did not report any outcomes that could provide usable data for the review, those which were quasi-randomized and those lacking a comparator arm.
We planned to extract data for the following outcomes, pre-defined by the Expert Working Group:
- Critical (primary for this review):
- Mortality (all-cause) – at 28-30 days, or in-hospital
- Progression to:
- Oxygen therapy
- Ventilation: non-invasive or invasive
- Critical or Intensive care (any reason) - Duration of hospitalization
- Need for hospitalization (for out-patients)
- Adverse events: all and serious
- Important (secondary):
- Time to clinical improvement
- Time to negative PCR for SARS-CoV-2
- Negative PCR for SARS-CoV-2 by day 7 post-enrolment
- Complications of COVID-19:
- Thrombotic events
- Pulmonary function/fibrosis
- Long covid/ post-covid sequalae
- Secondary infections
Two reviewers independently assessed eligibility of search results. One reviewer extracted data from each included study and assessed risk of bias using the Cochrane Risk of bias (RoB) v2.0 tool. Data and RoB assessments were checked against a Cochrane systematic review team’s extractions and assessments (we used a consensus approach). In case of any discrepancies, the whole RoB assessment was scrutinised by the whole team for this review, to reach consensus.
We used RevMan 5.4 to perform meta‐analysis using a random‐effects model for outcomes where pooling of effect estimates was appropriate. We used risk ratios (RR) for dichotomous outcomes and mean differences (MD) for continuous outcomes, with 95% confidence intervals (CIs). We planned to explore heterogeneity in the effect on mortality using subgroup analysis comparing between trials, based on COVID-19 illness severity of participants included and risk of bias. We used the I2 statistic to measure residual heterogeneity. We used GRADE methodology to assess the certainty in the evidence and documented this in a ‘Summary of findings’ table using GradeProGDT.
We included 20 trials involving 4140 participants, all of whom were adults, and 2122 of whom received ivermectin (1–20). Of these 11 studies are included in the previous recommendation and 9 new studies were added to update the evidence (21,22) While updating the evidence, we excluded 1 study (22) which was present in the previous analysis as it was retracted due to unreliable methodology. There were two trials each from, India, Iran, Pakistan, Brazil, and Mexico; one trial each was reported from Bangladesh, Colombia, Nigeria, Egypt, Israel, Italy, Argentina, Spain, Thailand, and Malaysia. Eleven were in hospitalized patients, four recruited out-patients only, one recruited both, and three did not report care setting. Disease severity, prevalence of comorbidities, and use of co‐interventions varied substantially between trials. The ‘Summary of characteristics of included trials’ table provides further details about the trials.
We found potential risks of bias across all domains; 12 of the 20 trials were at high risk of bias overall for at least one outcome. Risk of bias for each domain per trial is displayed alongside the Forest plots below. Studies excluded at full-text review are listed in the References section, with the reason provided in brackets (21,22,31–40).
The following comparisons were investigated in the trials. We compared outcomes for arms randomised to ivermectin vs. outcomes in arms with placebo, standard care, or agents considered inactive or ineffective against COVID-19. Where multiple arms contained ivermectin without another experimental agent, we combined results in those arms into a single ivermectin arm, but we did not double-count controls. Where another experimental agent undergoing investigation was combined with ivermectin, that trial arm was excluded from the analysis (e.g., doxycycline).
- Ten trials (3–5,8,9,11,14,17,18,20) compared ivermectin vs. placebo (2358 participants)
- Six [18;22-23;25-26;29] compared ivermectin vs. standard care (1244 participants)
- One (1) compared ivermectin vs. placebo vs. a combination of ivermectin & doxycycline in three arms (72 participants; 24 participants in ivermectin & doxycycline arm excluded)
- One (5) compared ivermectin vs. placebo vs. hydroxychloroquine in three arms (106 participants)
- One (2) compared ivermectin vs. lopinavir/ritonavir (62 participants)
- One (4) compared ivermectin vs. chloroquine or hydroxychloroquine (168 participants)
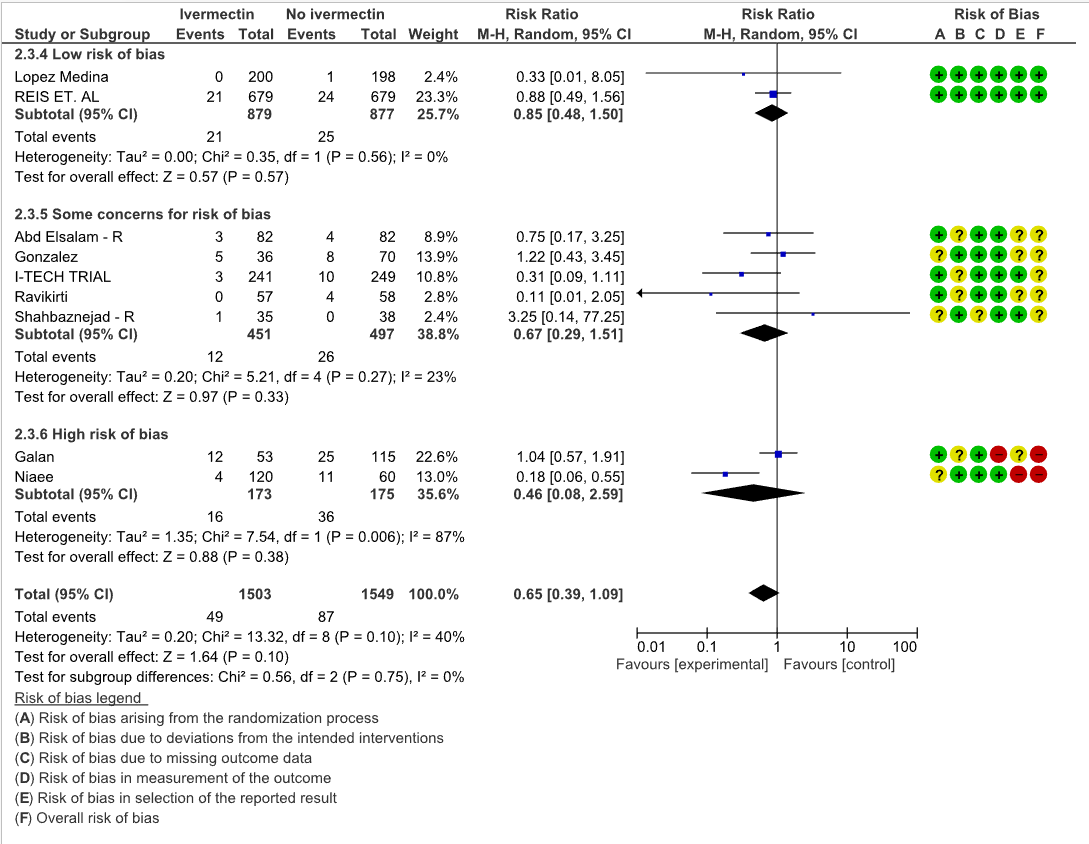
All-Cause-Mortality: Low certainty evidence from 9 RCTs (6,8,10,12,15,19,20) with 3052 participants shows that ivermectin may result in little to no difference in mortality [RR 0.65, 95%CI 0.39,1.09]. As the studies have some concerns and high risk of biases, a stratified analysis of the data was done based on ‘Risk of bias’. The trials (8,20) with Low risk of bias showed no difference in mortality in patients receiving Ivermectin vs no Ivermectin [RR 0.85, 95%CI 0.48,1.50]
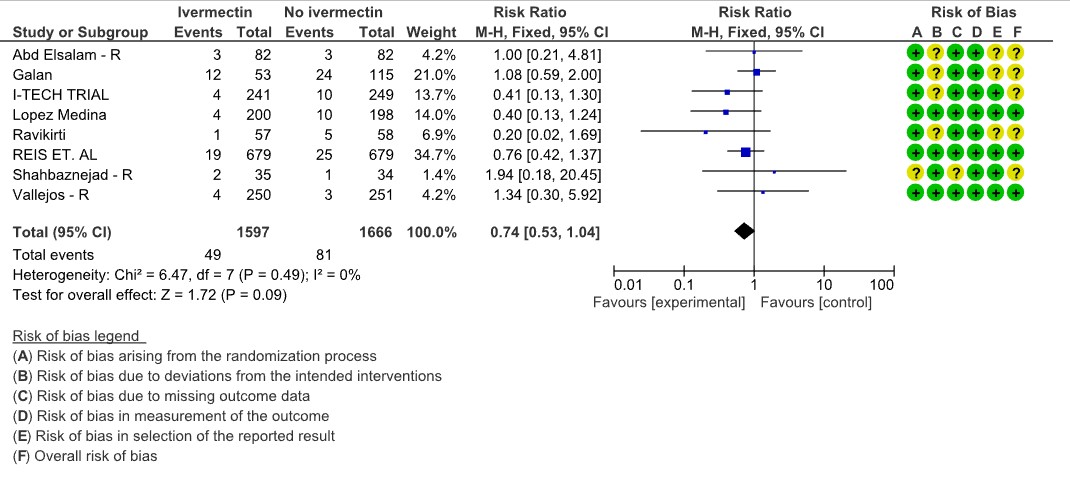
Progression to mechanical ventilation: Low certainty evidence from 8 trials (6,11,12,15,16) with 3263 participants showed that Ivermectin may have little to no effect in the progression to mechanical ventilation [RR 0.74, 95%CI 0.53,1.04]. 5 of the 8 included studies have some concerns.
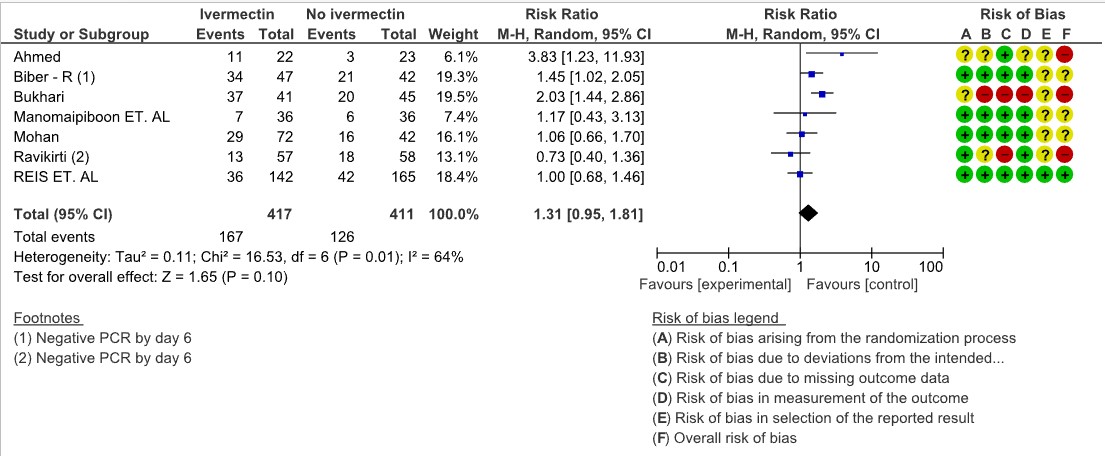
Negative PCR by day 7: Very low certainty evidence from 7 trials (1,3,11,13,17,20) with 828 participants for viral clearance at day 7 [RR 1.31, 95%CI 0.95,1.81] gives no impression of Ivermectin’s effect on viral clearance at Day 7. Of the 7 trials, 3 of them where of High Risk of bias, 3 of them had some concerns and only 1 trial with low risk of bias and had only 19% weightage. (Look at the forest plot).
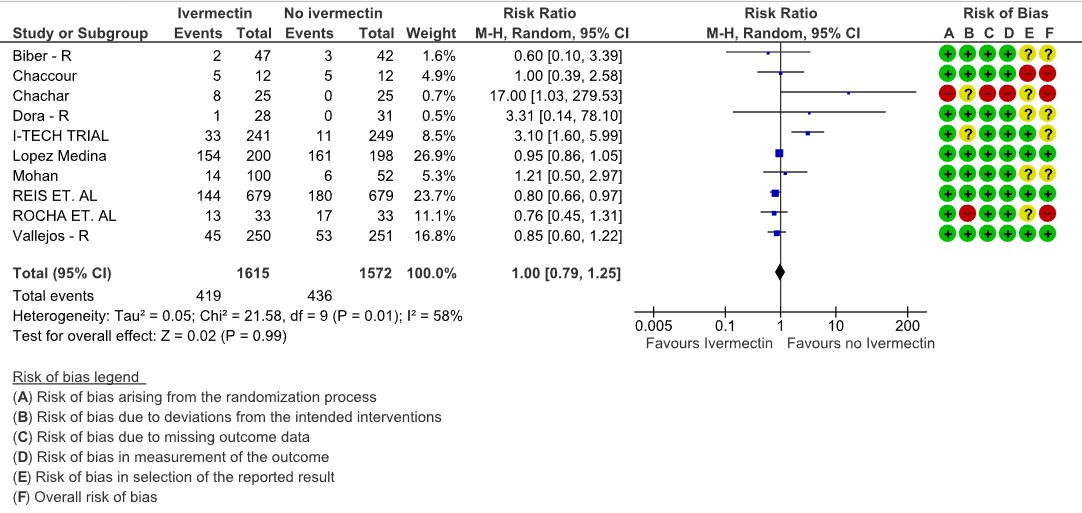
Adverse events: Low certainty evidence from 10 RCTs (4,5,8,9,13,14,16,18–20) with 3187 participants shows that Ivermectin results in no significant adverse events RR 1.00, [95%CI 0.79,1.25].
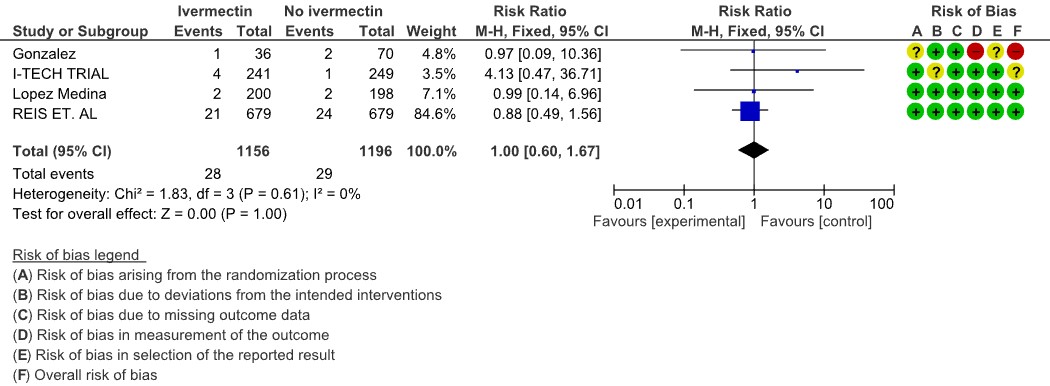
Serious adverse events: Low certainty evidence from 4 RCTs (7,8,19,20) with 2352 participants shows that Ivermectin results in no significant serious adverse events [RR 1.00, 95%CI 0.60,1.67].
One trial reported a higher risk of discontinuation of ivermectin vs. placebo due to an adverse event (RR 2.97; 95% CI 1.10 to 8.02; 1 trial (8); 398 participants).
95% confidence intervals for pooled effect estimates for all of the following outcomes not included in the summary of findings table included potential benefit and potential harm from ivermectin: need for critical or intensive care (2 trials (6,11); 283 participants); discharge from hospital by day 10 post-enrolment (1 trial (11); 115 participants); deterioration by 2 points on 8-point clinical ordinal scale (1 trial (8); 398 participants); lack of fever on day 7 (1 trial (1); 36 participants); lack of symptoms on day 7 (1 trial (5); 50 participants); and thrombotic events (1 trial (7); 106 participants). We were unable to pool data for time to clinical improvement as they were not reported in a way that was amenable to meta-analysis (3 trials (4,8,9); 149 participants).
No comparative data could be extracted for risk of progression to oxygen therapy; need for hospitalisation in outpatients; or post-acute COVID-19 pulmonary function/fibrosis or other sequelae; or secondary infections.
Lack of uniform criteria for COVID-19 severity, substantial overlap, and lack of clear reporting of severity in the included trials prevented a meaningful subgroup analysis by severity.
Furthermore, a lack of within trial comparison prevented subgroup analysis by age, duration of symptoms or dose of ivermectin. In addition, data of safety and efficacy in specific subgroups such as pregnancy, children, liver, and kidney disease were not available in the trials included in the rapid review.
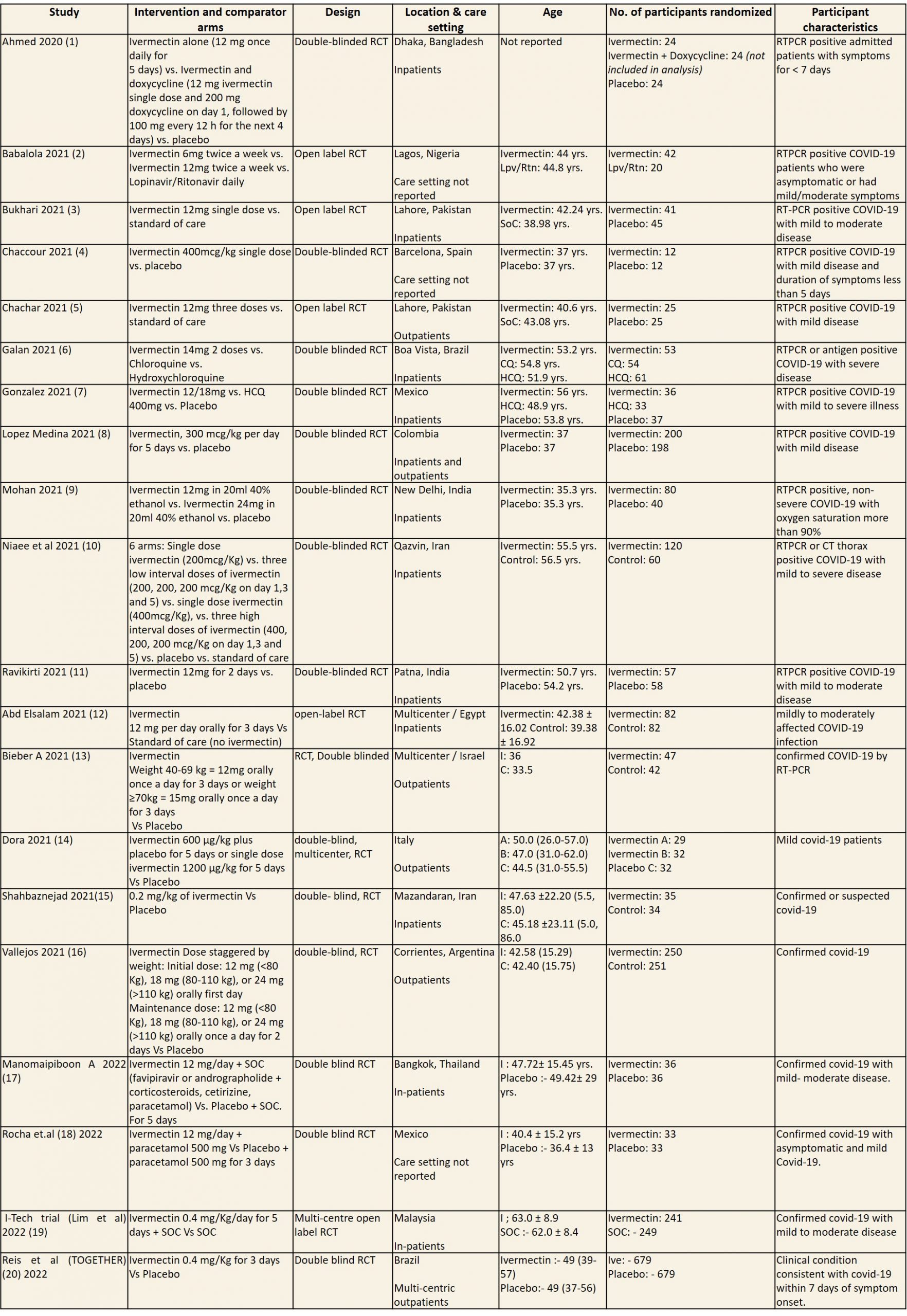
CQ: Chloroquine; ECOG: Eastern Cooperative Oncology Group score; HCQ: Hydroxychloroquine; Lpv/Rtn: Lopinavir/Ritonavir; NEWS: National early warning score; RCT: Randomized control trial; RTPCR: Reverse transcription polymerase chain reaction; SoC: Standard of care
1. Mortality, stratified by risk of bias
2. Progression to mechanical ventilation
3. Negative PCR for SARS-CoV-2 by day 7
4. Adverse events
5. Serious adverse events