COVID-19 infection contributes to a hypercoagulable state and thrombotic events are fairly common. Due to the frequency of arterial and venous thrombosis as well as microthrombosis demonstrated on lung histology, many clinicians all over the world have opted to use therapeutic anticoagulation in patients with severe or critical illness. In addition, there are numerous reports suggesting that the delta variant (B.1.617.2) now the predominant strain circulating widely in India results in many more thrombotic events and has also contributed to intrauterine deaths.
Overall among those with moderate, severe and critical COVID19, therapeutic dose anticoagulation appears to prevent clinically defined thrombotic events by 39%; RR=0.61 (95% CI 0.45-0.82) with moderate certainty of evidence. However it does not reduce mortality or organ support free days. It does however; seem to improve survival without organ support at 28 days by 6% [95% CI 1% to 10%].
When the moderate to severe group of patients were considered separately, the initiation of therapeutic anticoagulation also led to a decrease in thrombotic events by 37% (95% CI 7-57%), increase in Organ Support Free Days (OSFD) by 5% (95% CI 1 -10%), along with an increased risk of bleeding.
When the critical group was evaluated separately, therapeutic anticoagulation reduced thrombotic events by 43% (95% CI 11%-63%) with no decrease in all-cause mortality or OFSD. In addition there was no increase in bleeding RR 1.39 (95% CI 0.71 – 2.71). Due to the increasing evidence of thrombosis in all categories of patients, clinician discretion is required towards this category of patients. The group debated at length the advantages and disadvantages of therapeutic anticoagulation in this group. The group felt in the critical setting they are unable to pick up a thrombotic event easily which may impact eventual mortality and morbidity, and it is most often based on a clinical suspicion which are they are often unable to confirm as these patients are not amenable to easy shifting for a confirmatory radiology test. However the group felt it is easy to pick up major bleeding. In addition, fatal bleeding events which were reported only in the mpRCT (non-critical) were 3 in the therapeutic group as compared to 1 in the non-therapeutic group. Despite the uncertainty reflected in the various guidelines from NIH or NICE (refs) where due to the lack of data they are unable to recommend prophylactic over therapeutic, clinicians in the country are increasingly recommending an intermediate or therapeutic dose of anticoagulation in severe and critical categories. However, more trials are required to support the conclusion that therapeutic dose anticoagulation is beneficial in the moderate, severe and critical categories. The cost of the intervention is low and needs to be weighed against hospitalization and ICU care costs that may result due to a thrombotic event. However, there is no data on cost-effectiveness of the intervention at present.
Date of latest search: 9th June 2021.
Date of completion of Summary of findings table and presentation to Expert Working Group: 24th May and 9th June 2021.
Evidence synthesis team: Sushil S(SS), Jisha Sara John(JS), Richard Kirubakaran, Bhagteshwar Singh & Priscilla Rupali.
We acknowledge gratefully the assistance received from the authors of the multi-platform RCT[mpRCT] (ATTACC, ACTIV-4a, and REMAP-CAP platforms),specifically Ewan Goligher, who provided valuable assistance in evidence clarification and sharing of additional protocol documents.
Since December 2019, a worldwide pandemic labelled COVID-19, caused by SARS-CoV-2 virus has adversely impacted humanity in diverse ways (1). Clinical studies of hospitalized patients with SARS-CoV-2 initially showed flu-like symptoms, most commonly cough, sore throat, fever, myalgia, and fatigue at onset of COVID-19 illness, which can then proceed to develop into a viral pneumonia with varying severity (2-6).
Abnormal coagulation profiles and thrombotic complications, both venous and arterial, are common among the hospitalized severe and critically ill patients(7), with pulmonary embolism the most common site(8).
In addition, multiple autopsy reports show unprecedented pulmonary microvascular thrombosis and endothelial damage(9-12) which could be related to the direct viral cytopathic effect on the endothelial cells due to shared receptors with the alveolar cells(13). Other etiopathogenetic mechanisms include immune/cytokine mediated dysregulation of pro-coagulant & anti-fibrinolytic pathways.
Though hypercoagulability in COVID-19 has now been well-recognized, uncertainty still exists as to how best to manage clotting risk in these patients. In addition, an increased risk of hypercoagulability leading to increased thrombotic events have been reported and recognized extensively in the media and among peers. There is a prevailing assumption that the delta variant in India may be contributing to an increased number of thrombotic events, however this needs to be systematically studied and documented.
Over the past year several guidance documents have recommended the use of anticoagulation in hospitalized patients with COVID-19(14-17). Most of these guidelines recommend the use of unfractionated heparin (UFH) or low molecular weight heparin (LMWH), though the evidence is scarce with regard to which dose of anticoagulation i.e., prophylactic, intermediate, or therapeutic (full) dose should be employed in each severity strata of COVID19.
At present there is now fairly broad-based consensus, that the standard of care is prophylactic dose anticoagulation to all in-patients with COVID-19 pneumonia. However, it remains unclear if specific severity sub-groups of patients will benefit from intermediate or therapeutic dose anticoagulation in the absence of a confirmed thrombotic event.
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), Pubmed, MEDLINE, Epistemonikos(COVID Living Overview of Evidence platform), and the COVID‐19‐specific resource www.covid‐nma.com, for studies of any publication status and in any language published from March 2020 up to 15th April 2021. We also reviewed reference lists of systematic reviews and included studies.
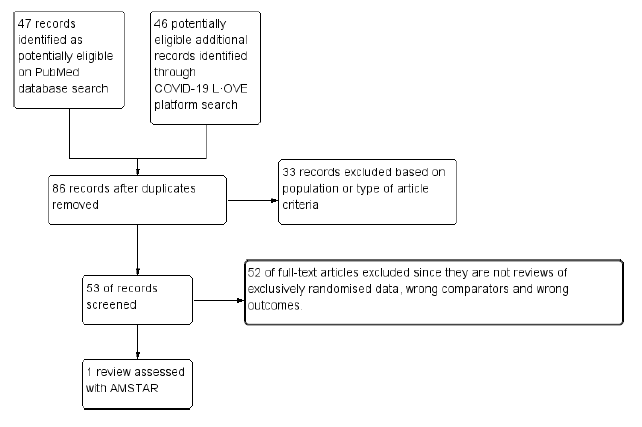
We searched the Pubmed database and found 47 systematic reviews, and from COVID Living Overview of Evidence(L*OVE) platform found 46 potentially eligible records. After removing duplicates, and excluding studies that did not include exclusively randomised control trial data or did not involve intended interventions, we found only one systematic review looking specifically at the outcome of mortality18. It was analysed with the AMSTAR 219 and was found to be of low quality of evidence and also did not look at most outcomes of interest, with regards to the PICO.
So we decided to proceed with a rapid review of available RCTs that compare between anticoagulation doses in COVID-19 patients.
We extracted data for the following outcomes, pre-defined by the Expert Working Group:
- Critical (primary for this review):
- Mortality (all-cause) – at 2-30 days, or in-hospital
- Thrombotic events
- Important (secondary):
- Time to clinical improvement
- Organ support free days(OSFD) :- ventilator, inotropic requirements.
- Survival without organ support at day 28
- Duration of hospitalization
- Bleeding events
On searching Pubmed & COVID L*OVE platform and when restricted to RCTs, we found 19 records. After excluding extraneous records and trials that did not report any outcomes that could provide usable data for the review, we were left with 5 RCTs which compared differing doses of anticoagulation in COVID-19 patients.
Two reviewers (SS & JSJ) independently assessed eligibility of search results. One reviewer extracted data from each included study, and both assessed risk of bias using the Cochrane Risk of bias (RoB) v2.0 tool20.
We used RevMan 5.421 to perform meta‐analysis using fixed & random‐effects models for outcomes where pooling of effect estimates was appropriate. We used risk ratios (RR) for dichotomous outcomes and mean differences (MD) for continuous outcomes, with 95% confidence intervals (CIs). Since the guidelines were going to be specific to each severity category we grouped studies as per their inclusion criteria into their severity categories and combined them as such to provide pooled estimates. We used the I2 statistic to measure residual heterogeneity. We used GRADE methodology22 to assess the certainty in the evidence, and documented this in a ‘Summary of findings’ table using GradeProGDT.
There are a myriad dosing strategies for anticoagulation based on indication, organ dysfunction, BMI and adverse drug reactions, based on available literature (23-25) and package insert recommendations(26). For purposes of our guidelines in the expert working group meeting it was decided to broadly specify doses - low & intermediate doses as non-therapeutic anticoagulation(1mg/kg IV once daily or ) AND as therapeutic dose anticoagulation(1mg/kg twice daily).
| Product | Thromboprophylaxis dose | Therapeutic dose | |
| Low dose | Intermediate dose | ||
| Low Molecular Weight Heparin(LMWH) - Enoxaparin | 40 mg q24h
[BMI>40/Weight >120 Kg – dose increase to 40 mg q12h] |
1 mg/kg q24h | 1mg/kg q12h |
| UnFractionated Heparin(UFH) | 5000U q12h | 5000 U q8h
OR 7500 U q12h |
80 U/kg bolus followed by 18 U/kg/hour infusion
Targeting APTT of 55-75 seconds |
Of the 6 RCTS found, three attempted to compare Therapeutic dose anticoagulation with non-therapeutic doses:
- HESACOVID :- compared prophylactic vs therapeutic dose of anti-coagulation (20 participants). 27
- mpRCT(Critically ill) pre-print: Zarychanski et al. is a collaboration of 3 RCT platforms, ACTIV-4a, REMAP-CAP and ATTACC, looking specifically at critically ill patients (total of 1074 participants) – comparing therapeutic vs non-therapeutic dose of anticoagulation28.
- mpRCT(Non-critically ill) pre-print:- Lawler et al. is a collaboration of above mentioned 3 RCT platforms, looking specifically at non-critically ill patients (total of 2291 participants) – comparing therapeutic vs non-therapeutic dose of anticoagulation29.
- COALITION ACTION: Looks specifically at the moderate-severe category of patients(34)
Two randomised trials studied the effect of intermediate Vs low dose thromboprophylaxis:
- INSPIRATION :- compared prophylactic Vs intermediate dose of anti-coagulation (562 participants)30.
- Usha Perepu et al, preprint :- compared prophylactic Vs intermediate dose of anti-coagulation (176 participants)31.
Since HESACOVID and the 2 RCTs recruiting patients from ATTACC, ACTIV-4a, and REMAP-CAP platforms(mpRCT critical) compared therapeutic vs non-therapeutic dose anticoagulation in the critical category of patients, they were analysed together. However, the mpRCT moderate and COALITION ACTION were analysed separately as well. The results of INSPIRATION and Usha Perepu et al were analysed separately in view of different comparator arms which were prophylactic and intermediate dose of anticoagulation.
The critical outcomes that were available and extracted for analysis from these studies included
- All-cause mortality (21-30 days),
- Thrombosis,
- Organ support free days [i.e., surviving to hospital discharge with reduced need for ICU-level organ support, including invasive and non-invasive mechanical ventilation]
- Survival without organ support at 28 days
- Major bleeding events.
Though we are using the term anticoagulation, the intent in all these trials was prophylaxis, but two different doses are being compared in each of these trials therapeutic vs non therapeutic which may be prophylactic or intermediate doses.
We included 4 trials with 3,927 patients of which 1 trial did not contribute much data (27). The two trials which did not include a therapeutic dose of anticoagulation as a comparator arm were excluded from this analysis (30,31). The patients were compared across different pre specified COVID19 severity groups, for the different outcomes as mentioned above (See summary of characteristics tables below). The duration of administration of anticoagulation varied from a minimum of 96 hours to 14 days or till the patient got better.
We tailored the severity strata in the study according to WHO COVID-19 Clinical management: living guidance severity classification (Interim document originally published under the title "Clinical management of COVID-19: interim guidance, 27 May 2020"(32).
| Study Group | WHO severity criteria correlate |
| mpRCT (Critically ill) - Zarychanski et al. | WHO Critical |
| mpRCT (non-Critically ill) - Lawler et al. | WHO Severe & Moderate |
The group of patients studied in the mpRCT(Critically ill) study28, correlated directly with WHO critical severity criteria. The group of patients studied in the mpRCT(non-Critically ill) study29, correlated with WHO severe category also overlapping with a few in the WHO moderate category.
Overall analysis: Using GRADE methodology certainty of evidence is shown in Summary of Findings tables.
- All-cause Mortality- Low certainty of evidence in 4 trials with 3927 patients, revealed that therapeutic dose anticoagulation may result in little to no difference in all-cause mortality, compared with non-therapeutic dose anticoagulation (RR 1.02, 95 % CI=0.82 to 1.27).
- Thrombosis- Moderate certainty of evidence in 4 trials with 3807 patients, revealed that therapeutic dose anticoagulation probably reduces thrombosis, when compared with non-therapeutic dose anticoagulation (RR= 61, 95 % CI = 0.45 to 0.82).
- Major bleeding- Moderate certainty of evidence in 3 trials with 3321 patients, revealed that therapeutic dose anticoagulation probably results in an increase in major bleeding, compared with non-therapeutic dose anticoagulation (RR 1.80, 95% CI = 1.13 to 2.86). There were 3 cases of fatal bleeds in mpRCT (non-critically ill) when given therapeutic dose anticoagulation vs 1 in the prophylactic dose anticoagulation.
- OSFD- Very low certainty of evidence in 2 trials with 3301 patients, revealed a very uncertain effect of therapeutic dose anticoagulation on organ support-free days in hospitalised patients, compared with non-therapeutic dose anticoagulation when patients from WHO moderate, severe & critical COVID19 strata were combined from available trials (RR=1.06,95%CI 0.72-1.56).
Since guidelines are to provide recommendations for each severity strata, disaggregated data was also assessed to provide analysis to help formulate recommendations specific to each severity strata.
Analysis according to severity strata
WHO Critical group: Very low certainty evidence from 2 trials (27, 28) showed that using therapeutic dose anticoagulation (TDA) did not significantly reduce mortality in critical COVID19 illness (RR-1.01, 95 % CI = 0.86 to 1.19). However, moderate certainty evidence did show decreased thrombosis in patients (RR-0.57, 95 % CI = 0.37 to 0.89) but with no increase in bleeding (RR-1.39, 95 % CI = 0.71 to 2.71). In addition, moderate certainty evidence from 1 trial (28), showed that therapeutic anticoagulation did not improve days free of organ support compared to prophylactic dose anticoagulation [Odds Ratio(OR) 0.87, 95% CI 0.70 to 1.08]. However, the median OSFD in the TDA group was 3 days vs 5 days in the PDA group. It was also noted that 41% received low dose PDA and 51% received an intermediate dose PDA.
Bayesian analysis from Zarychanski et al(28). showed a posterior probability of futility of 99.8% and posterior probability of inferiority of 89.4% for impact of therapeutic anticoagulation on OSFD. DSMB stopped recruitment in the same trial mpRCT severe group since pre-specified futility boundary for therapeutic anticoagulation was achieved33,however this was for OSFD, not for mortality or thrombotic events.
WHO Moderate/Severe group: Very low certainty evidence from 2 trials suggested that therapeutic anticoagulation provided no mortality benefit RR 1.02 (95% CI 0.79 to 1.30). However there was moderate certainty evidence that TDA did appear to prevent thrombosis by 37% (RR 0.63, 95 % CI 0.43 to 0.93) with a risk of major bleeding of about 19%; RR 2.25, 95 % CI 1.19 to 4.27).In addition there was moderate certainty evidence from 1 trial (29) showing that TDA increased the probability of OSFD with OR 1.05, 95 % CI 1.01 to 1.10 and similarly survival without organ support RR 1.06 (95% CI 1.01 to 1.10). However fatal bleeds in mpRCT (29) revealed 3 bleeds in TDA vs 1 in the PDA group.
Bayesian analysis from Lawler et al(29) gave a posterior probability of superiority of 99% for therapeutic anticoagulation improving OSFD. In the mpRCT (non-critical) group (29), deep venous thrombosis (DVT) was included as significant thrombosis which seems to have been excluded from mpRCT(critical)(28) group.
Analysis according to non-therapeutic doses
In a brief analysis of RCTs (INSPIRATION & Perepu et al.) which compared prophylactic vs intermediate dose anticoagulation (see table above), no statistically significant differences were noted in the outcomes of all-cause mortality [RR1.01,95% CI 0.84-1.21];thrombotic events [RR 1.17;95% CI 0.65-2.12];bleeding [RR 1.5;95%CI 0.82-2.71]; major bleeding [RR1.53;95%CI 0.55-4.26] assessed. (See relevant forest plot)
Add 2 table
The Anticoagulation Expert Working Group met on 24th May 2021 to consider the use of therapeutic Vs prophylactic dose anticoagulation in the management of COVID-19. A summary and then more detailed explanations of their judgements follow.
Summary of judgements – LOOKS DIFFERENT ONLINE
EtD summary table –
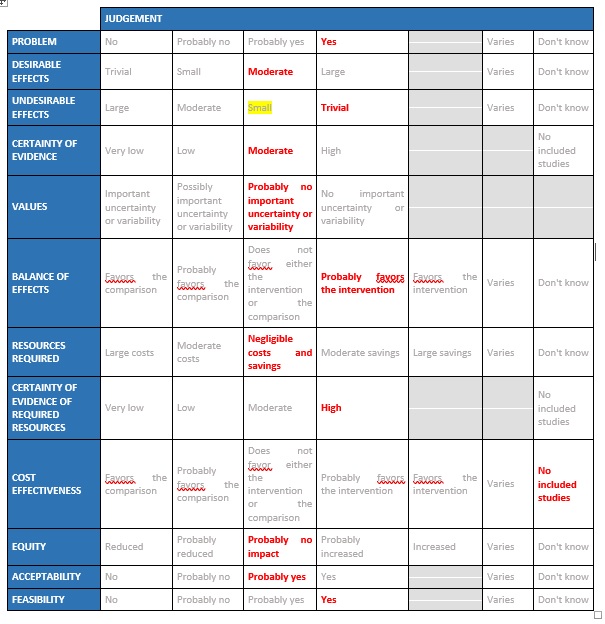
Problem
Hypercoagulability is a recognized phenomenon in COVID19 and is believed to be multifactorial. SARS CoV2 virus both directly and indirectly causes endothelial injury, microvascular inflammation, endothelial exocytosis, endothelitis contributing to acute respiratory distress syndrome. In post mortem studies microvascular occlusion with platelet-fibrin thrombi have been reported. In addition, changes in circulating prothrombotic factors and stasis due to immobility encountered in the critically ill has led to a recognized prothrombotic state in COVID19 infection, translating to increased arterial and venous thrombosis. This has led to the practice of prophylactic anticoagulation for all hospitalized COVID19 patients. However there exists an area of equipoise whether patients with severe or critical COVID19 infection will benefit with therapeutic (full dose) anticoagulation in the absence of a confirmed thrombotic event. This has especially become even more important as the country goes through a massive second wave probably caused by the delta variant B.1.617.2 starting in early February, which anecdotally seems to cause more thrombosis as per various reports in the media, however we need to await cohort studies for this to be accurately assessed.
Desirable effects
WHO Critical: At present, evidence shows that using TDA did not significantly reduce mortality in critical COVID19 but does appear to prevent thrombotic events by 42% (11-63%) with no statistically significant increase in bleeding with a moderate certainty of evidence. TDA also did not improve days free of organ support compared to PDA. DSMB stopped recruitment in this category as it felt that TDA did not offer any advantage towards OSFD (as a pre specified Bayesian post probability of futility was achieved). The group discussed this at length and felt that, preventing thrombosis was important even in the absence of mortality benefit. Panel also noted that most of the evidence was contributed to by the mPRCT with very few patients in HESACOVID.
WHO Moderate/Severe: The group noted that using TDA reduced thrombosis and increased the probability of OSFD but did not significantly reduce mortality or cause increased bleeding in moderate/severe category of COVID19. The group felt that right now thrombosis was an important event to prevent as it was difficult to recognize or confirm and probably would contributed to significant morbidity. However, the group felt that bleeding was easy to pick up and was rarely fatal. Hence the group that in an intensive care setting prevention of thrombosis was an important intervention. The various thrombotic events were reviewed and pulmonary embolism seemed to contribute to most of the events with other events recorded being myocardial infarction and strokes.
Undesirable effects
WHO Critical: The mPRCT (Critical) had around >500 patients in each arm and the incidence of bleeding in each group was similar. The actual difference in bleeding between the two groups was 1% suggesting that present evidence showed that the risk of bleeding was not increased. The DSMB of ACTIV-4 component of the mPRCT trial had recommended an early interim analysis to watch for the same, however the study was terminated as the futility threshold was reached suggesting that there was no benefit of TDA over PDA in the primary outcome of OSFD.
WHO Moderate/Severe: The mPRCT(Non critical) had around >1000 patients in each arm and the incidence of bleeding in the therapeutic dose group was slightly increased suggesting that in WHO moderate and severe COVID infection there seemed to be a mildly increased risk of bleeding.
The panel also discussed re the absence of data regarding anticoagulation in the mild and moderate groups without hypoxia and felt that decision re anticoagulation in those groups could be based on evidence from non-randomized studies and clinical experience.
Certainty of evidence
Overall the quality of evidence in the WHO moderate, severe and critical categories was felt to be moderate.
Values
Outcomes noted were considered to be important in overall patient management especially in setting of pandemic. The group felt that the outcomes of mortality, thrombotic events. Bleeding and Organ support free days were certainly important. They felt that there was no uncertainty or variability. However they did note some unusual points in the way outcomes were assessed.
Critical group: The group discussed the uncertainty as to whether thrombotic events could have contributed to mortality. There is no clear breakup of mortality in the pre-print or supplement. Clinically significant pulmonary embolism seems to have contributed to most of the thrombotic events, but it was not specified as to whether they were all major arterial or just segmental embolism. It also seemed unlikely that a patient who is severely or critically ill would have been shifted out for a CTPA. DVT was excluded in this group as a major thrombotic event.
Moderate: In the mpRCT (mod) group, Deep Venous Thrombosis was included as significant thrombosis which was excluded from mpRCT (critical) group.
Balance of effects
Given that the country is facing a shortage of beds, oxygen and intensive care units, if an intervention could reduce organ support and thrombosis it would be of benefit.
WHO Critical: There are very few trials overall to inform evidence and there seemed to be no mortality benefit or decrease in OSFD between TDA and PDA. There was a decrease in thrombotic events with no increase in bleeding noted. DSMB stopped the trial as futility end-point for OSFD was reached in interim assessment.
WHO Moderate/Severe: TDA appeared to increase OSFD, and prevent thrombotic events with a slightly increased risk for major bleeding. There was no mortality benefit between the 2 arms. OSFD should be given importance in the moderate category as it saves resources and prevents morbidity.
Resource requirements
There are likely to be negligible savings and costs pertaining to implementation of the TDA. Drugs used for this are relatively cheap, widely available and unlikely to incur a significant cost nor are they likely to result in significant savings. Health care workers in the country are fairly experienced with the use of the same and are aware of the various monitoring implications. Cost of implementation is low and needs to weighed against hospitalization and ICU care costs. Though monitoring of anticoagulation efficacy with Anti Xa testing will be possible only in an advanced hemostasis laboratory, if widely employed to ensure therapeutic efficacy it will likely also protect against unnecessary bleeding. However this will increase costs and probably unnecessary in most instances. There is also possible ineffectiveness of therapy in view of high rates of heparin resistance documented in published data but overall costs of implementing TDA are likely low if we are able to save on costs of hospitalisation and intensive care beds.
Certainty of evidence of required resources
Resources required for implementation of TDA are minimal and the certainty of evidence for this is high.
Cost effectiveness
At the moment there is no data regard to the cost effectiveness of this intervention and studies need to be done to be sure of the same. The group recognized the minimal costs and resources required to deliver as it is a subcutaneous injection which can be delivered by most HCWs easily. It is also likely that even if patients in the moderate category are given TDA, hospitalization will be dictated by disease severity rather than administration of anticoagulation, given that most health care settings and health professionals are comfortable with delivery of this intervention in the outpatient settings. There are also many novel oral anticoagulants available which have been proven to have similar efficacy as heparin and could potentially be employed as substitutes, however data with these are scarce in the COVID19 setting.
Equity
As the cost and requirements of anticoagulation delivery are reasonable, implementation can be equitable.
TDA is a feasible intervention which can be easily implemented in all health care settings by any health care professional.
There is anecdotal evidence that thrombotic risk is increased with the delta variant and this is increasingly being noticed in the second wave of COVID 19 in India. Whether this is more apparent due to the increased numbers or whether there is a true correlation of the delta variant with an increased risk of thrombosis remains to be determined. The working group felt that TDA in hospitalized patients with moderate disease (those who have progressively increasing O2 requirement) or severe disease might prevent thrombotic events, without any reduction in mortality. This subset might have increased probability of surviving to hospital discharge with reduced need for ICU-level organ support, including invasive and non-invasive mechanical ventilation (OSFD), with slightly increased risk for major bleeding.
However the group was less certain in the critical category of illness. The data shows a decrease in thrombotic events with no reduction of mortality or organ support free days and no increased risk of bleeding. The trial also reported a median in organ support days 3 vs 5 days in TDA and PDA respectively. Anecdotally most reported that they often give either intermediate or therapeutic doses routinely in their intensive care areas and felt that this decision should be individualized according to the clinical picture of the patient.
There is no evidence thus far that this dose is beneficial in mild, or in non-hospitalized patients.
Though there was no data regard to the cost effectiveness of this intervention, resources required for implementation of therapeutic anticoagulation are minimal in this subgroup of patients. This intervention is feasible to implement widely and easily. The evidence is for Injectable low molecular weight heparin only and not for Unfractionated Heparin or oral anticoagulants.
The subgroups of children <18 years of age, pregnant women, asymptomatic mild and out-patients were excluded from most studies. Some studies also excluded those on dialysis for chronic kidney disease, chronic liver and lung diseases as well as those on antiplatelet therapy.
The utility of D-dimer was also evaluated. In the mpRCT(non-critical) study it was noted that a high D-dimer is associated with a high risk of mortality and this was noted even in the mpRCT(non-critical) study, that participants with a high D-dimer were at increased risk of mortality and organ support and thus the adjusted absolute treatment benefits were more apparent. In the mpRCT – critical, the median D-dimer values were 827ng/ml in TDA vs 890 in the PDA group and about 48% of the patients in TDA vs 46% of PDA were noted to have a D-dimer twice the upper limit of normal.
There is no role for monitoring of D-dimer in non-hospitalised COVID 19 patients. A high D-dimer is known to be associated with an increased risk of venous thromboembolism in non covid patients and in Covid 19 infection it has been correlated with a poorer prognosis and increased mortality. However whether a high D-dimer value can be extrapolated to an increased risk of arterial or venous thrombosis in COVID19 infection is yet to be determined. Hence in hospitalized patients with COVID-19, there is insufficient data to recommend regular monitoring of D-dimer or base management strategies on the same.
In patients on therapeutic anticoagulation with unfractionated heparin, APTT monitoring can be done and maintained 1.5 to 2 times the control. In other anticoagulation regimens using low molecular weight heparin or Fondaparinaux, regular anti Xa monitoring is not recommended other than in obese patients. Anti Xa levels should be sent 3 hours after the dose of low molecular weight heparin. In the setting that heparin resistance is suspected, even in the setting of unfractionated heparin, anti Xa levels should be monitored. Target peak anti-Xa for the treatment doses of twice-daily enoxaparin is 0.6–1.0 IU/mL.
This conditional recommendation regarding use of anticoagulation may be revisited as evidence emerges. In addition to evidence of benefit, with its widespread use in India, there may be additional real-world reports regarding undesirable effects, which the group will monitor.
It has been shown that TDA may improve clinical outcomes in non-critically ill, but not critically ill COVID19 patients which seems counter intuitive though it can be explained away on the premise that critically ill patients are too far gone into the thromboinflammatory phase of illness where it may be futile. However, more studies are required to support a benefit with varying doses and in various subpopulation based on risk factors, comorbidities and utility of biomarkers like D-dimer. Studies also need to be done in mild and moderate COVID illness as to whether any form of anticoagulation can prevent progression of illness and/or hospital admission. Dose and duration of post discharge anticoagulation in the absence of a suspected or confirmed thrombotic event is another area where considerable equipoise exists. All of these are urgent research priorities considering the country is facing a manpower, oxygen, intensive care unit bed shortage.
- International Committee on Taxonomy of Viruses (ICTV). International Committee on Taxonomy of Viruses (ICTV) https://talk.ictvonline.org//taxonomy/p/taxonomy-history?taxnode_id=201851868.
- Chan, J. F.-W. et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. The Lancet 395, 514–523 (2020).
- Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet 395, 507–513 (2020).
- Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet 395, 497–506 (2020).
- Guan, W. et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 0, null (2020).
- Wang, D. et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 323, 1061–1069 (2020).
- Tang, N., Li, D., Wang, X. & Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 18, 844–847 (2020).
- Klok, F. A. et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. (2020) doi:10.1016/j.thromres.2020.04.013.
- Wichmann, D. et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19. Ann. Intern. Med. (2020) doi:10.7326/M20-2003.
- Ackermann, M. et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N. Engl. J. Med. 0, null (2020).
- Bradley, B. T. et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. The Lancet 396, 320–332 (2020).
- Polak, S. B., Van Gool, I. C., Cohen, D., von der Thüsen, J. H. & van Paassen, J. A systematic review of pathological findings in COVID-19: a pathophysiological timeline and possible mechanisms of disease progression. Mod. Pathol. 33, 2128–2138 (2020).
- Hoffmann, M. et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 181, 271-280.e8 (2020).
- Bikdeli, B. et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 75, 2950–2973 (2020).
- Thachil, J., Cushman, M. & Srivastava, A. A Proposal for Staging COVID‐19 Coagulopathy. Res. Pract. Thromb. Haemost. rth2.12372 (2020) doi:10.1002/rth2.12372.
- Moores, L. K. et al. Prevention, Diagnosis, and Treatment of VTE in Patients With Coronavirus Disease 2019: CHEST Guideline and Expert Panel Report. Chest 158, 1143–1163 (2020).
- Cuker, A. et al. American Society of Hematology 2021 guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19. Blood Adv. 5, 872–888 (2021).
- Ongoing Living Update of Potential COVID-19 Therapeutics Options Summary of Evidence. Rapid Review (6th May 2021).
- Shea, B. J. et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358, j4008 (2017).
- Cochrane Handbook for Systematic Reviews of Interventions. /handbook/current.
- RevMan. /online-learning/core-software-cochrane-reviews/revman.
- GRADEpro. https://gradepro.org/.
- Rocca, B. et al. Antithrombotic therapy and body mass: an expert position paper of the ESC Working Group on Thrombosis. Eur. Heart J. 39, 1672–1686f (2018).
- Rosovsky, R. P. et al. When Pigs Fly: A Multidisciplinary Approach to Navigating a Critical Heparin Shortage. The Oncologist 25, 334–347 (2020).
- Eck, R. J. et al. Intermediate Dose Low-Molecular-Weight Heparin for Thrombosis Prophylaxis: Systematic Review with Meta-Analysis and Trial Sequential Analysis. Semin. Thromb. Hemost. 45, 810–824 (2019).
- Lovenox (enoxaparin sodium) [package insert]. Bridgewater, NJ: Sanofi; December 2018.
- Lemos, A. C. B. et al. Therapeutic versus prophylactic anticoagulation for severe COVID-19: A randomized phase II clinical trial (HESACOVID). Thromb. Res. 196, 359–366 (2020).
- Remap-Cap, T., ACTIV-4a, Investigators, A. & Zarychanski, R. Therapeutic Anticoagulation in Critically Ill Patients with Covid-19 – Preliminary Report. medRxiv 2021.03.10.21252749 (2021) doi:10.1101/2021.03.10.21252749.
- The ATTACC, A.-4a et al. Therapeutic Anticoagulation in Non-Critically Ill Patients with Covid-19. medRxiv 2021.05.13.21256846 (2021) doi:10.1101/2021.05.13.21256846.
- INSPIRATION Investigators et al. Effect of Intermediate-Dose vs Standard-Dose Prophylactic Anticoagulation on Thrombotic Events, Extracorporeal Membrane Oxygenation Treatment, or Mortality Among Patients With COVID-19 Admitted to the Intensive Care Unit: The INSPIRATION Randomized Clinical Trial. JAMA 325, 1620–1630 (2021).
- Perepu, U. et al. Standard Prophylactic Versus Intermediate Dose Enoxaparin in Adults with Severe COVID-19: A Multi-Center, Open-Label, Randomised Controlled Trial. https://papers.ssrn.com/abstract=3840099 (2021) doi:10.2139/ssrn.3840099.
- WHO Clinical management of COVID-19: interim guidance, 27 May 2020.
- mpRCT interim presentation.pdf. Available online at https://nhlbi-connects.org/documents/mpRCT%20Interim%20Presentation.pdf.
- Lopes DR, de Barrose Silva PGM, Furtado RH et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID19 and elevated D-Dimer concentration (ACTION): an open label,multicentre, randomised controlled trial. https://doi.org/10.1016/ S0140-6736(21)01203-4
Covid Management Guidelines India Group - Anticoagulation Working Group. Prophylactic Vs Therapeutic dose anticoagulation. Covid Guidelines India; Published online on June 9, 2021; URL: https://indiacovidguidelines.org/anti-coagulation/ (accessed ).
